Olaf Kahl, Vanda Vatslavovna Pogodina, Tatyana Poponnikova, Jochen Süss and Vladimir Zlobin
Key Points
- TBE virus is a flavivirus and a prominent tick-borne human pathogen occurring in parts of Asia and Europe.
- The virus was discovered by Lev A. Zilber and co-workers in the former USSR during an expedition in the Far Eastern taiga under the most difficult conditions in 1937.
- They and members of a second expedition under the leadership of the Academician Evgeny N. Pavlovsky 1938 elucidated the basic eco-epidemiology of the virus.
- In their natural foci, TBE virus circulates between vectors, certain ixodid ticks, and some of their hosts, so-called reservoir hosts, mostly small mammals.
- Five different subtypes of TBE virus have been described to date.
Introduction
Tick-borne encephalitis virus (TBEV) is an arthropod-borne human pathogen, ecologically known as an arbovirus.1 Taxonomically, it is a member of the genus Flavivirus together with other medically relevant arboviruses (e.g., Yellow fever virus, Dengue virus). The virus is endemic in Asia and Europe where it circulates between its principal vectors, usually hard ticks of the genus Ixodes, and certain small mammals, referred to as ‘reservoir hosts’, fed on by virus-infected vector ticks. The bite of infected vector ticks is also the common route of infection for humans. Each year several thousand people fall ill with TBE. Long before Smith and Kilbourne2 discovered that ticks can transmit pathogens to their hosts and before TBEV was discovered, the disease had been mentioned in the literature. Parish records from the Åland islands (Finland) contain case descriptions of a disease at least similar to TBE in the 18th century.3 ‘Taiga encephalitis’ or ‘biphasic meningoencephalitis’ had been observed in eastern parts of the former USSR mostly in soldiers, railway workers and loggers, as the region began to develop in the 19th century.
Schneider4 was the first to give a medical description of the ‘Epidemische akute Meningitis serosa’ (also known as ‘Schneidersche Krankheit’ in Austria), which was in fact TBE. Panov5 gave the first detailed description of the clinical picture of the so-called ‘summer encephalitis’ in the Far East.
This chapter presents a brief synopsis of the major milestones in TBE and TBEV research, beginning with the discovery of the virus in the former USSR.
Discovery of TBEV in different regions of Eurasia
Molecular biological data indicate that TBEV has its origins in Western Siberia approximately 3100 [1800–4900] years ago.6 From there the eastern TBEV groups spread to the east through Asia and the western TBEV groups to the west, and they might have reached central Europe approximately 2000 years ago. However, the first isolation of TBEV succeeded only in 1937.
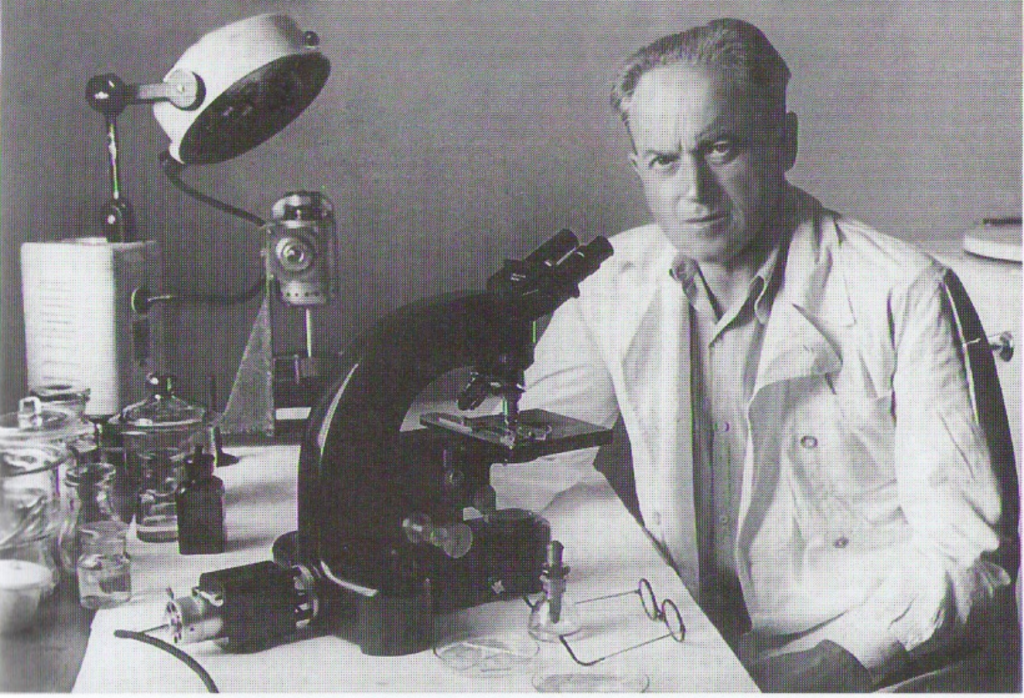
In the 1930s, a large number of people living in the taiga in the Far East and Soviet troops located in that region fell ill with a serious neurological disease, with a frequently fatal outcome. The etiology of the disease was unknown, and first attempts to identify the pathogen failed. In 1937, the USSR Ministry of Health sent out an expedition, which was led by Lev A. Zilber, the head of the first medical virological laboratory in the country. Zilber put together a group of very capable and highly motivated young researchers and technical assistants. They worked in two teams at two different remote places in the taiga under extremely difficult conditions. The northern team was working in the Khabarovsk Territory (leader: Elizabeth N. Levkovich) and the southern team in Primorsky Territory (leader: Alexandra D. Sheboldaeva). No infrastructure for scientific research existed in the area of the taiga where the disease occurred, so the teams had to find simple, practical solutions for establishing what they called a scientific campus.
The teams started their practical work in mid-May 1937, and very soon the first relevant results were available. When investigating local people, they found numerous cases with neurological symptoms. Twelve out of 64 hospitalized patients died.
The virus was isolated from 29 febrile patients, from diseased mice (after they had been infected with a tick suspension), and from ticks feeding on them. When team members warned local people to avoid tick bites, the number of new cases distinctly decreased. So there was compelling evidence at the end of that mission in mid-August that the team had found the causative viral agent, with Ixodes persulcatus ticks as the vectors.
written by his son L.L. Kisselev and E.S. Levina, published in 2005
by the publishing house “Science” in the series “Scientific biographies”
Unfortunately, some team members became infected with TBEV and developed disease symptoms. Fortunately, nobody died – which appears almost unavoidable when taking into consideration the highly unsafe conditions and the highly contagious nature of the virus. As an example, Dr. Chumakov, who became a famous virologist later on, fell ill with a severe form of TBE after cutting his finger during the autopsy. Residual effects were right-arm paralysis and hearing loss. However, this did not prevent him from finding new TBEV foci in the Ural and Transural regions, far away from the Far East.7
Scientifically, the expedition was a great success. Zilber and the other team members had isolated the causative virus, elucidated the basic eco-epidemiology of the disease, and provided some effective prophylactic information on how to avoid an infection. Further expeditions were sent out to the Far East to learn more about the virus and the disease and its prophylaxis.8
The first cases of TBE in China were reported in 1943, and the causative virus was isolated in 1944 from brain samples of patients who had died (reviewed in Yoshii et al., 2017).9 The discovery of TBE in Europe started with the clinical-epidemiological description of 24 cases of aseptic meningitis in the district of Neunkirchen (Lower Austria) by Schneider in 1931.4 Although the outcome was described as benign, the convalescence of many patients was prolonged. In the early 1940s scientists of the Rockefeller Institute for Medical Research in New York showed serological cross-reactions between hyperimmune sera of Louping ill virus and Russian Spring Summer encephalitis virus.
The first documented TBEV isolation in Europe was made from Ixodes ricinus ticks (strain 256) in Belarus in 193910, and the second isolation was reported in former Czechoslovakia in 1948 (strain Hanzalova, isolated near Prague).11 In 1952, a virus strain (KEM I) was isolated during an alimentary outbreak in Hungary. Other eastern European countries followed shortly after, and TBEV strains were isolated in Slovenia in 1953, in Poland in 1954, in Austria in 1954 (strain Scharl), and in Slovakia in 1958. The first TBEV strain in Finland was detected in 1959 (Kumlinge strain).12 Sweden reported the first detection of TBEV in 1954, and Denmark reported the first clinical cases of TBE from Bornholm Island, also in the 1950s. In Norway, however, the first described human case of TBE occurred only in 1997.14 In Germany, the first descriptions of TBE and the first virus isolations resulted from the late 1950s in the former German Democratic Republic.15 Rehse-Küpper et al. (1978)16 were probably the first who isolated TBEV strains in the former Federal Republic of Germany as the two virus strains isolated by Müller et al. (1970) were to the best of our knowledge never confirmed as being TBEV.17
France followed with the first isolation of TBEV from the Alsace region in 1970.18 It was only in 2016 that the first autochthonous human cases of TBE were described in The Netherlands and a TBEV strain (strain
Salland) was detected in ticks.19
Credit: LJ Bruce-Chwatt from the Wellcome Collection
The detection of the TBEV natural transmission cycle
Due to the pioneering research work by the Zilber expedition in the Far East, the basic outlines of TBEV eco- epidemiology were elucidated within a few months in 1937. They found that the pathogen is a virus that can be transmitted through the bite of Ixodes persulcatus, a hard tick (family Ixodidae).
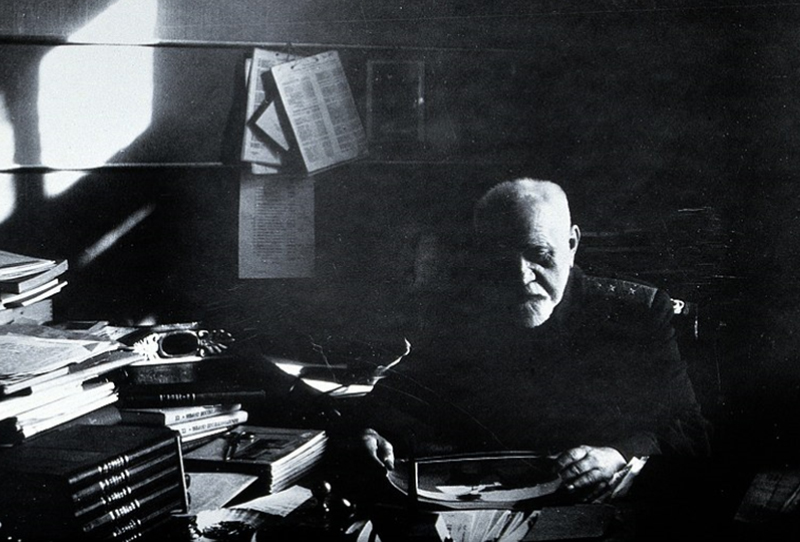
Another expedition was sent out by the USSR Ministry of Health to the Far East under the leadership of E.N. Pavlovsky in 1938 to learn about the circulation of TBEV in the field and the involved reservoir hosts. Largely based on the findings during that expedition, Pavlovsky20,21 developed the famous concept of ‘The Natural Nidality of Transmissible Diseases’, where he described the ecology of zoonoses. Arthropod vectors (ixodid ticks) that become infected with TBEV through a blood meal on an infective host carry the virus to the following life stage(s) and transmit it during the following blood meal(s) to a host. So-called reservoir hosts become infected through the bite of an infected tick, and in turn transmit the virus to other feeding ticks. Long-term virus circulation exists only in definite types of landscape with suitable abiotic conditions where all the necessary biotic partners (vectors, reservoir hosts) are present in sufficient densities.
Chumakov & Naidenova22 (cited after23) found the hard tick Ixodes ricinus, a close relative of I. persulcatus, to be a vector of a milder form of TBE in some European areas of the former USSR. This was later confirmed by various European researchers. Rampas & Gallia24 from Czechoslovakia were the first outside the former USSR to isolate TBEV from field-collected ticks.
An alternative alimentary route of human TBE infection became apparent in the European part of the former USSR from 1947 to 1951.25 Groups of people contracted TBE after consuming unpasteurized goat milk or goat milk products (e.g., cheese) from viremic goats. Similar alimentary TBE epidemics occurred also in other TBE endemic countries, e.g., in Rožňava (south-eastern Slovakia) with more than 600 cases in 195123 and in Niesky (former German Democratic Republic) in 1961.26
Field work on TBEV decreased in several European countries in the 1970s and 1980s. TBEV ecology seemed to be well understood. The main interest of researchers focused more on the molecular biology of TBEV and also on the newly discovered Borrelia burgdorferi, the causative agent of human Lyme borreliosis. Interestingly, this coincided with the first European TBE vaccine becoming available in 1976,27 and the TBE problem seemed to be solved.
Jones et al.28 made the significant finding in the laboratory that guinea pigs can infect feeding Rhipicephalus appendiculatus with Thogoto virus, another tick-borne virus, without showing an apparent viremia. Encouraged by this finding, Alekseev & Chunikhin29 and Labuda et al.30 demonstrated non-viremic transmission of TBEV from small mammals (infected through tick bite) to uninfected feeding ticks. This was a major step forward in our understanding of the field ecology of the virus, and reactivated interest in TBEV ecology. Milan Labuda and various co-workers made a number of further relevant contributions to this topic.31-33 They found (i) that TBEV is transported in Langerhans’ cells in infected hosts, (ii) that non-viremic transmission also occurs in immune hosts, and (iii) that this kind of transmission happens in small, but not in larger mammals. The most commonly used term now is ‘co-feeding transmission’, although non-viremic transmission might technically be the better term.
The detection of different TBEV subtypes
Based on general viral properties such as viral morphology, physical and chemical properties, virion structure, arthropod carriers, and serological cross-reactions, the genus Flavivirus including TBEV was considered to be part of the family Togaviridae. This term was first offered by Lwoff and Tournier (1966).34 The family Togaviridae consisted of the genera Alphavirus (former arbovirus group A), Flavivirus (former arbovirus group B) with Dengue virus, type 1, and some other viruses.35,36
De Madrid and Porterfield37 divided the genus Flavivirus into 7 subgroups according to plaque reduction neutralization test (PRNT). The first subgroup includes tick-borne viruses such as TBEV, Omsk hemorrhagic fever virus, Louping ill virus, Langat virus, Negishi virus, and Kyasanur forest disease virus. Along with the above-mentioned viruses, the TBEV complex included Alma Arasan, Apoi, Royal-Farm, Kadam, Powassan viruses, and according to Gaidamovich and Loginova38 also Gadgets Gully, Saumarez Reef, Karshi, and Tyuleniy viruses.
These viruses share some antigenic similarity but have different geographic distributions, associations with different ticks and vertebrate hosts, and a different pathogenic potential for humans. Due to a difference in the replication strategies of alpha- and flaviviruses, the family Flaviviridae was established as an independent family that comprises the genus Flavivirus with more than 70 species dividing into 10 serocomplexes.39 According to modern classification, the family Flaviviridae comprises the genera Flavivirus, Pestivirus, and Hepacivirus. TBEV belongs to the mammalian tick-borne flavivirus group and comprises 3 subtypes: European, Far Eastern, and Siberian.40
Two geographic and antigenic variants of TBEV (Eastern and Western) had been known for 40 years.1,41-44 Clarke43 divided 28 strains in 2 antigen variants by the gel precipitation test with cross-absorbed sera. She concluded that there are 2 antigen subtypes: Eastern and Western (Central European). Chumakov et al.45 considered that Eastern and Western subtypes differ within the species TBEV; they proposed a classification into ‘Persulcatus’ and ‘Ricinus’ antigen variants according to viral ecology. Votyakov et al.44,46 argued that the infectious agents of Eastern and Western TBE are different species according to differences in antigen profiles, geography, clinical and pathological features in animals and humans.
Pletnev et al.47,48 and Mandl et al.49,50 decoded the complete genomes of Eastern (Sofjin) and European (Neudoerfl) strains and thereby started a new phase of intraspecific TBEV classification. The obtained data proved that the genetic differences between the Western and Eastern variants are significant with 16.8–16.9% of nucleotide substitutions and 6.9–7.2% of amino acid substitutions. Two Eastern strains in contrast have 3- and 4-times lower differences in nucleotide (4.6%) and amino acid (1.8%) substitutions, respectively.
Rubin and Chumakov51 published the first results of the Siberian subtype. They demonstrated some peculiarities of the strain Aina isolated in the Irkutsk region, USSR, from a child with TBE. Pogodina et al.52,53 described a group of strains isolated in Eastern Siberia from I. persulcatus, from rodents and patients serologically closely related to the strain Aina. Gritsun et al.25,54 were the first to genotype strains of the Siberian subtype by gene E and complete genome sequencing. Two strains – Vasilchenko (L40361) and Zausaev (AF527415) – became prototype strains of 2 Siberian subtype clusters (reflecting their geographic localization).
Sequencing a gene E fragment (160 bp length) of 8 and thereafter 29 strains isolated in different geographic regions, carried out by Zlobin et al.55-57 enabled the identification of 3 major genotypes (subtypes): (1) Far Eastern, (2) Western, and (3) Ural-Siberian (Siberian). According to Ecker,58 TBEV consists of 3 subtypes corresponding to 3 major genotypes: European, Far Eastern, and Siberian.
However, Grard59 reinterpreted the data of the genetic relationships among arthropod-borne viruses. She suggested that TBEV should include 4 subtypes: (1) Louping ill virus (Spanish, British, and Irish subtypes), (2) TBEV (European subtype), (3) TBEV (Far Eastern and Siberian subtype), and (4) Turkish sheep encephalitis virus and its subtype, Greek goat encephalitis virus.
Beside the 3 described and accepted subtypes, 2 different strains – 178/79 and 886/84 – have been described by Russian researchers. These 2 strains have been shown not to be closely related to any of the 3 known subtypes.60 Additional studies are needed to demonstrate whether these strains can be classified as new TBEV subtypes. These results mean also that further TBEV subtypes may be detected in future.
Acknowledgement:
We are most grateful to Jeremy Gray who helped improve the manuscript.
Contact:
Citation:
Kahl O, Pogodina VV, Poponnikova T, Süss J, Zlobin VI. A short history of TBE. Chapter 1. In: Dobler G, Erber W, Bröker M, Schmitt HJ, eds. The TBE Book. 6th ed. Singapore: Global Health Press; 2023. doi:10.33442/26613980_1-6
References
- Casals J. Viruses: the versatile parasites; the arthropod-borne group of animal viruses. Trans N Y Acad Sci. 1957;19:219-35.
- Smith T, Kilbourne FL. Investigations into the nature, causations and prevention of Texas or southern cattle fever. Bureau Anim Ind Bull. 1893:322pp.
- Kunz C, Heinz FX. Tick-borne encephalitis. Vaccine. 2003;21Suppl 1:S1-2.
- Schneider H. Über epidemische akute Meningitis serosa. Wiener Klin Wochenschr. 1931;44:350-2.
- Panov AG. Klinika vesenne-letnikh entsefalitov. Nevropat I Psikhiat. 1938;7:18-32.
- Heinze DM, Gould EA, Forrester NL. Revisiting the clinal concept of evolution and dispersal for the TB flaviviruses by using phylogenetic and biogeographic analyses. J Virol. 2012;86:8863-71.
- Chumakov MP, Seitlenok NA. Tick-borne human encephalitis in the European part of USSR and Siberia. Science. 1940;92:263-4.
- Zlobin VI, Pogodina VV, Kahl O. A brief history of the discovery of TBE virus in the late 1930s (based on reminiscences of members of the expeditions, their colleagues, and relatives). Ticks Tick-Borne Dis. 2017;8:813-20.
- Yoshii K, Song JY, Park SB, Yang J, Schmitt HJ. Tick-borne encephalitis in Japan, Republic of Korea and China. Emerg Microbes Infect. 2017; 6(9):e82
- Chumakov MP. Tick-borne encephalitis in humans. PhD of Med. Sci. Moscow, 1944 (In Russian).
- Gallia F, Rampas J, Hollender L. Laboratory infection with encephalitis virus. Cas Lék Ces. 1949;88:224-229 (in Czech.).
- Oker-Blom N, Kääriäinen L, Brummer-Korvenkontio M, Weckström P. Symp. Czech. Acad. Sci. 1962;3:423. (cited after Brummer-Korvenkontio et al., 1973)
- Brummer-Korvenkontio M, Saikku P, Korhonen P, Oker-Blom N. Arboviruses in Finland. I. Isolation of tick-borne encephalitis (TBE) virus from arthropods, vertebrates, and patients. Am J Trop Med Hyg. 1973;22:382-9.
- Skarpaas T, Ljøstad U, Sundøy A. First human cases of tickborne encephalitis, Norway. Emerg Infect Dis. 2004;10:2241-3.
- Sinnecker H. Zeckenencephalitis in Deutschland. Zbl Bakt., I. Abt Orig. 1960;180:12-18.
- Rehse-Küpper B, Danielová V, Klenk W, Abar B, Ackermann R. The isolation of Central European encephalitis (Tick-borne encephalitis) virus from Ixodes ricinus (L.) ticks in southern Germany. Zbl Bakt Hyg., I. Abt Orig. A 1978;242:148-155.
- Müller W, Löffler S, Preis B. Experimentelle Untersuchungen über das Vorkommen von Arboviren in Unterfranken. II. Charakterisierung zweier Virusstämme. Zentralbl Bakteriol Orig. 1970;214:465-479.
- Hannoun C, Chatelain J, Krams S, Guillon JC, Lepine P. Isolement, en Alsace, du virus de l’encephalite à tiques (Arbovirus, groupe B). C R Acad Sci Paris. 1971;272:766-8.
- de Graaf JA, Reimerink JH, Voorn GP, et al. First human case of tick-borne encephalitis virus infection acquired in the Netherlands, July 2016. Euro Surveill. 2016;21.
- Pavlovsky EN. On the natural focality of infectious and parasitic diseases. Vestn. Akad. Nauk SSSR 1939;10:98–108. (in Russian)
- Pavlovsky EN. Natural Nidality of Transmissible Diseases: With Special Reference to the Landscape Epidemiology of Zooanthroponoses. University of Illinois Press; 1966.
- Chumakov MP, Naidenova GA. The tick Ixodes ricinus as a vector of the tick-borne (spring-summer) encephalitis. Med Parazitol. Parazit Bolezni. (Moscow) 1944;4:89-93 (In Russian).
- Blaškovič D. The public health importance of tick-borne encephalitis in Europe. Bull WHO. 1967;36(suppl 1):5-13.
- Rampas J, Gallia F. The isolation of encephalitis virus from Ixodes ricinus. Cas Lek Ces. 1949;88:1179-1180.
- Gritsun TS, Lashkevich VA, Gould EA. Tick-borne encephalitis. Antiviral Res. 2003;57:129-46.
- Helpert A, Sinnecker H. Ausgewählte Erhebungen zur Zeckenenzephalitis-Epidemie im Kreis Niesky, Bezirk Dresden, 1961. Deutsch Gesundheitsw. 1966;21:1277-9.
- Kunz C. Vaccination against TBE in Austria: the success story continues. Int J Med Microbiol. 2002;291 Suppl 33:56-7.
- Jones LD, Davies CR, Steele GM, Nuttall PA. A novel mode of arbovirus transmission involving a nonviremic host. Science. 1987;237:775-7.
- Alekseev AN, Chunikhin SP. The exchange of the tick-borne encephalitis virus between ixodid ticks feeding jointly on animals with a subthreshold level of viremia. Parazit Bolezni. (Moscow). 1990:48-50. (In Russian)
- Labuda M, Jones LD, Williams T, Danielova V, Nuttall PA. Efficient transmission of tick-borne encephalitis virus between cofeeding ticks. J Med Entomol. 1993;30:295-9.
- Labuda M, Austyn JM, Zuffova E, et al. Importance of localized skin infection in tick-borne encephalitis virus transmission. Virology. 1996;219:357-66.
- Labuda M, Kozuch O, Zuffova E, Eleckova E, Hails RS, Nuttall PA. Tick-borne encephalitis virus transmission between ticks cofeeding on specific immune natural rodent hosts. Virology. 1997;235:138-43.
- Nuttall PA, Labuda M. Tick-borne encephalitis subgroup. In: Ecological Dynamics of Tick-borne Zoonoses. Eds Sonenshine DE, Mather TN: Oxford University Press; 1994;pp.351-391.
- Lwoff A, Tournier P. The classification of viruses. Annu Rev Microbiol. 1966;20:45-74.
- Fenner F, McAuslan BR, Mims CA. The Biology of Animal Viruses. New York – London: Academic Press; 1974.
- Horzinek M. Togaviruses. Ann Med Vet. 1978;122:293-9.
- De Madrid AT, Porterfield JS. The flaviviruses (group B arboviruses): a cross-neutralization study. J Gen Virol. 1974;23:91-6.
- Gaidamovich SY, Loginova NV. Family Togaviridae. In: General and Particular Virology, Moscow: Medicina. 1982;2:520pp (In Russian).
- Westaway EG, Brinton MA, Gaidamovich S, et al. Flaviviridae. Intervirology. 1985;24:183-92.
- Thiel H-J, Collett MS, Gould EA, et al. Family Flaviviridae. In: Virus Taxonomy: Classification and Nomenclature. Eighth Report of the International Committee on the Taxonomy of Viruses. Eds Fauquet CM, et al. Amsterdam: Elsevier; 2005;979-996.
- Chumakov MP. Investigations on ultraviral encephalitides. VI. Transmission of tick-borne encephalitis virus to the progeny of ixodid ticks and the problem of natural reservoirs of this infection. Med Parazit (Moscow). 1944;6:38 (In Russian).
- Clarke DH. Antigenic analysis of strains group B arthropod- borne viruses by antibody absorption. J Exp Med. 1960;1: 21- 32.
- Clarke DH. Further studies on antigenic relationships among the viruses of the group B tick-borne complex. Bull WHO. 1964;31:50-66.
- Votyakov VI, Protas II, Zhdanov VM. Western tick-borne encephalitis. Minsk: Belarus; 1978;255 pp. (In Russian).
- Chumakov MP, Rubin SG, Linev MB. Three antigen types of tick-borne encephalitis virus, their dependence on arthropod vectors and geography. Problems of Medical Virology (Мoscow). 1975:371-5 (In Russian).
- Votyakov VI, Zlobin VI, Mishayeva NP. Tick-borne encephalitis of Eurasia: Ecology, Molecular epidemiology, Nosology and Evolution. Novosibirsk Nauka. 2002 (In Russian).
- Pletnev AG, Yamshchikov VF, Blinov VM. Tick-borne encephalitis virus genome. The nucleotide sequence coding for virion structural proteins. FEBS Lett. 1986;200:317-21.
- Pletnev AG, Yamshchikov VF, Blinov VM. Nucleotide sequence of the genome and complete amino acid sequence of the polyprotein of tick-borne encephalitis virus. Virology. 1990;174:250-63
- Mandl СW, Heinz FX, Kunz C. Sequence of the structural proteins of tick-borne encephalitis virus (western subtype) and comparative analysis with other flaviviruses. Virology. 1988;166:197-205.
- Mandl СW, Heinz FX, Stocke E, Kunz C. Genomic sequence of tick-borne encephalitis virus (western subtype) and comparative analysis of nonstructural proteins with other flaviviruses. Virology. 1989;173:291-301.
- Rubin SG, Chumakov MP. New data on the antigenic types of tick-borne encephalitis (TBE) virus. Zentralbl Bakteriol. 1980;Suppl. 9:231-6.
- Pogodina VV, Bochkova NG, Levina LS, et al. Immunological and some etiology aspects of the Aina/1448 serotype of tick- borne encephalitis virus. Voprosy Virusol. 1981;6:735-41 (In Russian).
- Pogodina VV, Bochkova NG, Koreshkova GV. Properties of strains of tick-borne encephalitis virus, Aina/1448 serotype. Voprosy Virusol. 1981:741-5 (In Russian).
- Gritsun TS, Frolova TV, Pogodina VV, Lashkevich VA, Venugopal K, Gould EA. Nucleotide and deduced amino acid sequence of the envelope gene of the Vasilchenko strain of TBE virus; comparison with other flaviviruses. Virus Res. 1993;27:201-9.
- Zlobin VI, Mamayev LV, Dzhioev YP, Kozlova IV. Genetic types of tick-borne encephalitis virus. J Infect Pathol (Irkutsk) 1996;3:13-7 (In Russian).
- Zlobin VI, Demina TV, Belikov SI, et al. Genetic typing of tick- borne encephalitis virus based on an analysis of the levels of homology of a membrane protein gene fragment. Voprosy Virusol. 2001;1:16-21 (In Russian).
- Zlobin VI, Demina TV, Mamayev LV, et al. Analysis of genetic variability of strains of tick-borne encephalitis virus by primary structure of a fragment of the membrane protein E gene. Voprosy Virusol. 2001:13-6 (In Russian).
- Ecker M, Allison SL, Meixner T, Heinz FX. Sequence analysis and genetic classification of tick-borne encephalitis viruses from Europe and Asia. J Gen Virol. 1999;80:179-85.
- Grard G, Moureau G, Charrel RN, et al. Genetic characterization of tick-borne flaviviruses: new insights into evolution, pathogenic determinants and taxonomy. Virology. 2007;361:80-92.
- Demina TV, Dzhioev YP, Verkhozina MM, et al. Genotyping and characterization of the geographical distribution of tick- borne encephalitis virus variants with a set of molecular probes. J Med Virol. 2010;82:965-76.