Song Joon Young
E-CDC status: imperiled – unknown if affected or endemic
(no new data available as of May 2023)
History and current situation
Although no human case of tick-borne encephalitis (TBE) has been documented in South Korea to date,5 surveillance studies have been conducted to evaluate the prevalence of tick-borne encephalitis virus (TBEV) in wild ticks.1-5 Four studies collected ticks by dragging or flagging in grassland and forest, while 1 study tested wild mammals (boars and rodents) by removing ticks from them. In the wild of South Korea, Haemaphysalis spp. were the predominant species found by tick dragging, while Ixodes nipponensis became predominant when harvested from small mammals.6
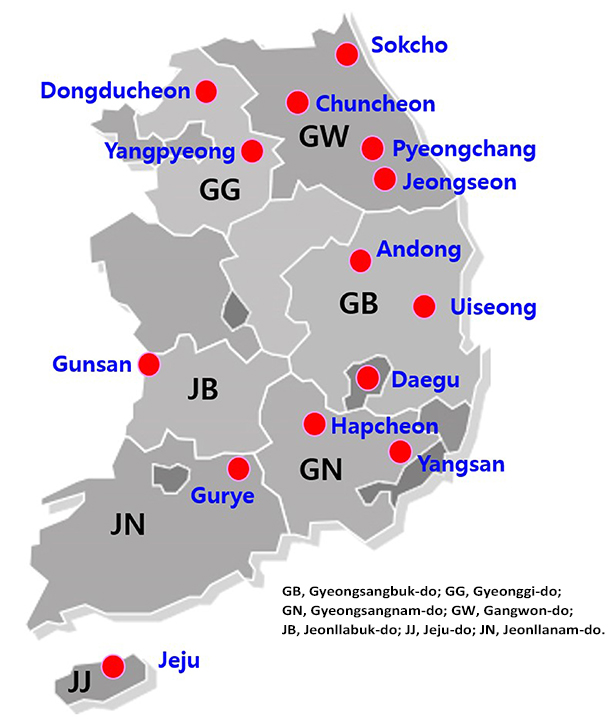
According to the results, TBEV was detected in numerous regions (Figure 1):
- Gyeonggi-do (Yangpyeong and Dongducheon),
- Gangwon-do (Pyeongchang, Jeongseon, Sokcho, and Chuncheon),
- Jeonllabuk-do (Gunsan and Gurye),
- Gyeongsangbuk-do (Hapcheon, Dongu, Andong, and Uiseong),
- Gyeongsangnam-do (Yangsan), and
- Jeju-do (Jeju).1-5
The first study was conducted in 12 regions of 5 provinces of South Korea in 2005–2006.1
TBEV was detected from Haemaphysalis longicornis (minimum field detection rate, 0.2%), H. flava (0.8%), H. japonica (0.9%), and I. nipponensis (1.6%), as depicted in Table 1.
The minimum field detection rate ([number of detection positive pools/ total number of examined ticks] × 100) was particularly high in Yangpyeong (5.9%–20.0%), Dongducheon (1.3%–6.7%), Pyeongchang (0.8%–1.3%), and Jeongseon (0.4%–8.3%) with variation by tick species. As usual, 1–30 ticks were included in each pool. Phylogenetic analysis revealed that the TBEV in South Korea belonged to the Western subtype, contrary to neighboring countries including Japan, China, and northeastern Russia, where the Far-Eastern subtype was only isolated (Table 1).
In the second study by the same research team, TBEV was also isolated from wild rodents (Apodemus agrarius) captured in Hapcheon, Gyeongsangnam-do.2 These TBEV isolates (KrM216, KrM219) caused symptoms of encephalitis in suckling mice and were able to grow from brain preparations in cell culture. In 2007, the third TBEV surveillance was conducted in the southern provinces of South Korea, including Jeju Special Self-Governing Province (Jeju Island), Jeollanam-do, Gyeongsangbuk-do, and Gyeongsangnam-do.3 Among the 6,788 ticks collected, 4,077 were pooled (649 pools) by collection site. In Jeju Island, the minimum field detection rate was 0.17% in H. longicornis and 0.14% in H. flava. In accordance with the previous study, the Jeju strains were identified as Western subtype TBEV by phylogenetic analysis.
Later during 2011–2012, the fourth larger-scale surveillance study was carried out in 25 localities of 10 provinces of South Korea.4 A total of 13,053 ticks were collected with H. longicornis as the most abundant species (90.8%, 11,856/13,053), followed by H. flava (8.8%, 1,149/13,053), I. niponensis (0.3%, 42/13,053), and Ixodes persulcatus (0.05%, 6/13,053). The minimum field detection rate for H. longicornis, H. flava, and I. nipponensis were 0.06%, 0.17%, and 2.38%, respectively, and the TBEV sequences obtained were identified as the Western subtype, consistent with the previous reports.1–3
In 2014, the most recent surveillance study was conducted to evaluate the prevalence of TBEV and other tick-transmitted viruses (Powassan virus, Omsk hemorrhagic fever virus, Langat virus, and severe fever with thrombocytopenia virus) among wild ticks.5 A total of 21,158 ticks were collected by dragging at 139 sites in 6 provinces; H. longicornis was the dominant tick species (83.04%, 17,570/21,158), while other tick species, H. flava (15.68%, 3317), I. nipponensis (1.18%, 249), Amblyomma testudinarium (0.05%, 11), and H. phasiana (0.04%, 8), were much less common. TBEV was detected by nested reverse transcriptase-polymerase chain reaction (RT-PCR) in the Andong, Uiseong, Daegu, and Yangsan areas. The maximum likelihood estimation (estimated numbers of viral RNA-positive ticks per 1,000 ticks) for H. longicornis, H. flava, and I. nipponensis was 0.23%, 0.90%, and 8.02%, respectively. On phylogenetic analysis, the TBEV strains identified in this study belonged to the Western subtype also.
Even though no confirmed human TBE case was reported in South Korea, TBEV might have been endemic in various localities and H. longicornis, H. flava, and I. nipponensis would be potential vectors of the Western subtype TBEV.
Overview of TBE in South Korea
In South Korea, TBE is designated as a group 4 Nationally Notifiable Infectious Disease, requiring immediate reporting for laboratory-confirmed cases.8
Although no case of TBE has been confirmed in South Korea, human encephalitis cases with unknown causes have been increasingly reported. TBE screening at the Korean Centers for Disease Control and Prevention (KCDC) was started in 2006. As for undefined encephalitis cases or suspected TBE cases, blood and cerebrospinal fluid (CSF) samples are required to be sent out to KCDC to perform enzyme-linked immunosorbent assay (ELISA) and RT-PCR for TBEV. However, there are significant limitations of TBEV clinical surveillance in South Korea. First, TBE disease awareness is quite low, and diagnostic practice is limited in clinical settings. Neurologists often take care of undefined meningitis/encephalitis cases, but they are completely unfamiliar with TBE. Second, considering the short duration of TBE viremia, it is not easy to confirm the infection using blood and CSF samples collected at later clinical stages. To better characterize the disease burden of TBE in South Korea, serologic studies are required to evaluate TBE prevalence in high-risk populations such as forest workers and farmers in the endemic areas. At the same time, active surveillance with enhanced awareness would be essential to find missed TBE cases.
As of May 2023, no human cases of TBE have been reported.9
| Table 1: Virus, vector, transmission of TBE in South Korea | |
|---|---|
| Viral subtypes, distribution | Western subtype1-5 |
| Reservoir animals | Wild rodent (Apodemus agrarius) |
| Infected tick species (%) | H. longicornis, H. flava, H. japonica, and I. nipponensis |
| Dairy product transmission | Not documented |
| Table 2: TBE-reporting and vaccine prevention in South Korea | |
|---|---|
| Mandatory TBE reporting | Yes: TBE is a group 4 Nationally Notifiable Infectious Disease in South Korea7
Case definition: laboratory-confirmed patient
|
| Other TBE-surveillance | None |
| Special clinical features | No information available |
| Available vaccines | Not available |
Figure 1: Geographical locations where TBEV-positive ticks or wild rodents were identified in South Korea
Acknowledgments
Updates for 6th Edition provided by Eugine Yang, Medical & Scientific Relations, Vaccines Medical Affairs, Pfizer.
Contact:
infection@korea.ac.kr
Citation:
Song JY. TBE in South Korea. Chapter 12b. In: Dobler G, Erber W, Bröker M, Schmitt HJ, eds. The TBE Book. 6th ed. Singapore: Global Health Press; 2023. doi:10.33442/26613980_12b31-6
References
- Kim SY, Jeong YE, Yun SM, Lee IY, Han MG, Ju YR. Molecular evidence for tick-borne encephalitis virus in ticks in South Korea. Med Vet Entomol. 2009;23:15-20.
- Kim SY, Yun SM, Han MG, et al. Isolation of tick-borne encephalitis viruses from wild rodents, South Korea. Vector Borne Zoonotic Dis. 2008;8:7-13.
- Ko S, Kang JG, Kim SY, et al. Prevalence of tick-borne encephalitis virus in ticks from southern Korea. J Vet Sci. 2010;11:197-203.
- Yun SM, Song BG, Choi W, et al. Prevalence of tick-borne encephalitis virus in ixodid ticks collected from the republic of Korea during 2011-2012. Osong Public Health Res Perspect. 2012;3:213-21.
- Yun SM, Lee YJ, Choi W, et al. Molecular detection of severe fever with thrombocytopenia syndrome and tick-borne encephalitis viruses in ixodid ticks collected from vegetation, Republic of Korea, 2014. Ticks Tick Borne Dis. 2016;7:970-8.
- Ree HI. In: Medical Entomology: Medical Arthropodology. 4th ed. Seoul: Komoonsa; 2005:345-90.
- Yoo SJ, Park JH. Necessity of a Surveillance System for Tick-borne Encephalitis. Osong Public Health Res Perspect. 2017;8:155.
- Korean Centers for Disease Control and Prevention. Case Definitions for National Notifiable Infectious Diseases; 2016.
- Korea Disease Control and Prevention Agency. Guideline on the Management of Tick- and Rodent-Borne Infections. KDCA. Accessed May 8, 2023. https://www.kdca.go.kr/filepath/boardSyview.es?bid=0019&list_no=722023&seq=1