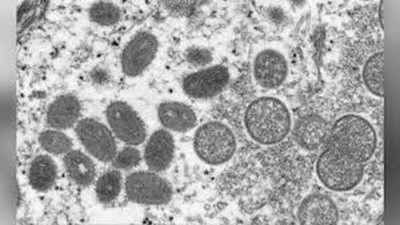
 Scientists at the Centers for Disease Control and Prevention (CDC) are collaborating with the Massachusetts Department of Public Health to investigate a case of monkeypox in a Massachusetts resident who had recently traveled to Canada by private transportation. Testing in Massachusetts found orthopox virus infection on May 17, 2022, and CDC labs confirmed as monkeypox.
Scientists at the Centers for Disease Control and Prevention (CDC) are collaborating with the Massachusetts Department of Public Health to investigate a case of monkeypox in a Massachusetts resident who had recently traveled to Canada by private transportation. Testing in Massachusetts found orthopox virus infection on May 17, 2022, and CDC labs confirmed as monkeypox.
CDC is also tracking multiple clusters of monkeypox that have been reported within the past two weeks in several countries that don’t normally report monkeypox, including Portugal, Spain, and the United Kingdom. It’s not clear how people in those clusters were exposed to monkeypox but cases include individuals who self-identify as men who have sex with men. CDC is urging healthcare providers in the U.S. to be alert for patients who have rash illnesses consistent with monkeypox, regardless of whether they have travel or specific risk factors for monkeypox.
Monkeypox was first discovered in 1958 when two outbreaks of a pox-like disease occurred in colonies of monkeys kept for research, hence the name “monkeypox.” The first human case of monkeypox was recorded in 1970 in the Democratic Republic of Congo during a period of intensified effort to eliminate smallpox. Since then, monkeypox has been reported in humans in other central and western African countries.
Anyone, regardless of sexual orientation, can spread monkeypox through contact with body fluids, monkeypox sores, or shared items (such as clothing and bedding) that have been contaminated with fluids or sores of a person with monkeypox. Monkeypox virus can also spread between people through respiratory droplets typically in a close setting, such as the same household or a healthcare setting. Common household disinfectants can kill the monkeypox virus.
“Many of these global reports of monkeypox cases are occurring within sexual networks. However, healthcare providers should be alert to any rash that has features typical of monkeypox. We’re asking the public to contact their healthcare provider if they have a new rash and are concerned about monkeypox,” said Inger Damon, MD, PhD, a poxvirus expert with more than 20 years’ experience and Director of CDC’s Division of High-Consequence Pathogens and Pathology, where the agency’s poxvirus research is based.
What healthcare providers should do:
- If healthcare providers identify patients with a rash that looks like monkeypox, consider monkeypox, regardless of whether the patient has a travel history to central or west African countries.
- Some patients have had genital lesions and the rash may be hard to distinguish from syphilis, herpes simplex virus (HSV) infection, chancroid, varicella zoster, and other more common infections.
- Isolate any patients suspected of having monkeypox in a negative pressure room, and ensure staff understand the importance of wearing appropriate personal protective equipment (PPE) and that they wear it each time they are near suspected cases.
- Consult the state health department or CDC’s monkeypox call center through the CDC Emergency Operations Center soon as monkeypox is suspected.
Monkeypox is a rare but potentially serious viral illness that typically begins with flu-like illness and swelling of the lymph nodes and progresses to a widespread rash. Within 1 to 3 days after the appearance of fever, the rash develops usually beginning in the face then spreading to other parts of the body. Lesions progress through the following stages before falling off: macules, papules, vesicles, pustules, and scabs. The illness typically lasts for 2–4 weeks. In Africa, monkeypox has been shown to cause death in as many as 1 in 10 persons who contract the disease.
By Dr. Simone Müschenborn-Koglin Contributing Editor, GHP