 A 3rd death has been linked to a Mycobacterium chelonae outbreak at Cambridge’s Royal Papworth Hospital, England. A 26-year-old patient underwent a double lung and heart transplant in June 2019. The patient tested culture positive for M. chelonae following the surgery and continued to suffer devastating complications. He died in July 2021, still testing positive for M. chelonae.
A 3rd death has been linked to a Mycobacterium chelonae outbreak at Cambridge’s Royal Papworth Hospital, England. A 26-year-old patient underwent a double lung and heart transplant in June 2019. The patient tested culture positive for M. chelonae following the surgery and continued to suffer devastating complications. He died in July 2021, still testing positive for M. chelonae.
A spokesperson for Royal Papworth Hospital NHS Foundation Trust said: “In February 2022, a coroner had launched an investigation into the 2020 deaths of a 54-year-old patient, and a 60-year-old patient, both had been infected with Mycobacterium abscessus, a different organism. A total of 21 patients were infected, 5 of whom had received transplants. As part of our extensive investigations, we have put multiple measures in place to maintain safety, including treatment of the water supply and installing special filters on taps and showers which our regular testing shows is effective.”
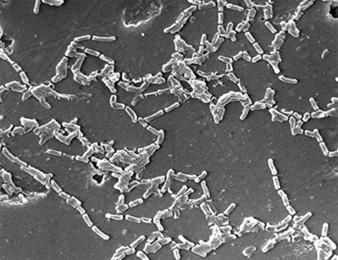
Mycobacterium abscessus and M. chelonae are both acid-fast bacilli belonging to the non-tuberculous mycobacteria (NTM) complex. NTMs are environmental mycobacteria, found in natural and potable freshwater and soil. NTM can form biofilms on the inner surfaces of water distribution systems, which are resistant to chlorine.
M. chelonae is one of the most pathogenic rapidly growing mycobacteria (RGM). In immunocompetent patients, the most common clinical scenario is localized skin infections, infection after an invasive procedure, or catheter-related infection. Pulmonary infections due to M. chelonae are rare, but colonization is common in cystic fibrosis patients. Disseminated and invasive infections are seen in immunocompromised patients. Person to person transmission has not been documented. Cervical lymphadenitis in children is rare. Mycobacterium avium intracellulare and Mycobacterium haemophilum are more frequently associated with cervical lymphadenitis in children compared to M. chelonae.
M. chelonae is not macrolide-resistant and does not have an erythromycin methylase (erm) gene so macrolides are effective for treating M. chelonae infections, whereas they are generally not effective for M. abscessus infections because most isolates have an active erm gene.
Unlike M. chelonae, M. abscessus is a pulmonary pathogen. Infections with M. abscessus are usually treated with a combination therapy of amikacin, tigecycline, cefoxitin, and imipenem, combined with oral clarithromycin or azithromycin (if the patient’s isolate is macrolide susceptible), for one month, followed by a combination of clofazimine, linezolid, minocycline, moxifloxacin, or co-trimoxazole for 12 months, depending on results of susceptibility testing.
Further investigation on this outbreak is currently ongoing.
See the guidelines from the US Cystic Fibrosis Foundation (CFF) and the European Cystic Fibrosis Society (ECFS).
By Dr. Simone Müschenborn-Koglin Contributing Editor, GHP