In science fiction, we see all kinds of nightmare viruses that evolve immunity to vaccinations. The scary part? It could actually happen in real life, especially if anti-vaxxers encourage people not to get vaccinated. Populations with pockets of non-vaccinators are more likely to evolve vaccine-resistant viruses than populations where everybody gets a vaccination.
In science fiction, we see all kinds of nightmare viruses that evolve immunity to vaccinations. The scary part? It could actually happen in real life, especially if anti-vaxxers encourage people not to get vaccinated. Populations with pockets of non-vaccinators are more likely to evolve vaccine-resistant viruses than populations where everybody gets a vaccination.
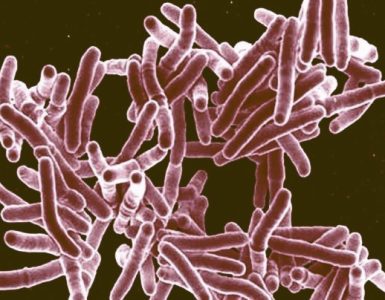
Viruses are still around because, like everything else that wants to stay alive, they’re always changing. As our bodies come up with new immune responses, they mutate and keep coming at us. These slight mutations are called antigenic drift, and they’re the reason why we have to keep getting new flu vaccinations every year. The flu virus gets into the body and uses its protein configurations to bind to receptor sites, generally on lung cells — unless a person’s existing antibodies can stop them. When the flu mutates, the existing antibodies won’t work anymore, and so we develop new ones. With any luck, we develop them before we die of the flu. Vaccines are meant to prompt antibodies that can bind to the flu virus, and give us the immune response we need without the bother of getting sick. But if our immune system can react to the flu faster, won’t that drive the flu to mutate faster? Not necessarily.
To a certain extent, vaccines do prompt antigenic drift in viruses. When a group of people are immune to a particular configuration of a virus, they leave the playing field open to any newly-produced virus that has just a slightly different configuration. There’s not much competition, as the original virus is quickly dealt with by vaccinated hosts.
The people carrying the slightly mutated virus, however, move freely though a population that has no immunity — what’s called a “naive” population. For a virus to produce mutated “offspring,” it needs to have fertile ground in which to reproduce. In order to make lots of second-generation viruses, one of which may be a useful mutant, the virus needs to have a lot of infected people manufacturing its babies. When an entire population is immune to a flu virus, it can’t reproduce enough to have a good chance of offspring with a useful mutation. Life doesn’t always find a way — just look at smallpox.
But low vaccination rates also contribute to antigenic drift in a different way. This was discovered when researchers at the National Institute of Allergy and Infectious Diseases started giving mice the flu. The mice were separated into two groups; one group received vaccines for a strain of flu, and the other did not. After the mice were infected with the flu, their lung tissue was checked for signs of the virus, and then used to infect the next group of mice.
After nine repetitions of the process, researchers compared the virus from the vaccinated mice and the virus from unvaccinated mice. The unvaccinated mice produced a virus that had not appreciably changed. The virus from the vaccinated mice had mutated slightly. It clung a little more tightly to the receptor cells on the lungs, allowing it to duck the antibodies that would destroy its chances of infection. The scientists called this a high-affinity virus, because of its affinity for the cell’s receptor, then stuck that virus in unvaccinated mice again. The virus promptly reverted to its low-affinity form.
This might make it look like vaccines drive antigenic drift, but it’s not that simple. For one thing, the virus wasn’t responding to a vaccine, but to antibodies. A population-wide flu epidemic would have leave the population in the same state as a population-wide vaccination program, except with a great deal more dead bodies. There was also a reason why, as soon as the antibody pressure was off, the virus reverted to its low-affinity form. If the flu virus clings too tightly to the receptor, it sacrifices its ability to move from cell to cell, spreading the infection. High-affinity isn’t superpower. It is, quite possibly, an evolutionary end point.
It’s not, however, the final twist. In this model for the virus, it alternates between populations with a number of antibodies (either from vaccines or from previous viruses), and naive populations. Its ability to change between high-affinity and low-affinity configurations gives it legs, and it travels through the population, adding on more mutations and more resistance. It’s the alternation that drives the drift, and a poorly-vaccinated population provides the chance for alternation.
The researchers recommend fighting this model for antigenic drift by eliminating the “naive” population. Keeping a group up-to-date on their vaccinations — especially children, who haven’t been exposed to many types of the flu — will reduce the chance that the virus will be handed back and forth between the exposed and the naive populations. Keeping vaccination rates high can stop us from needing new vaccinations.
Source: io9.com