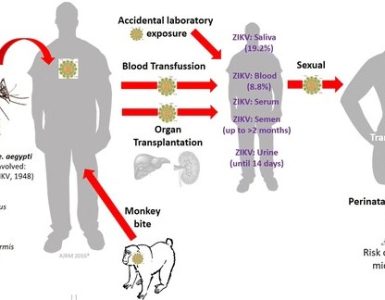
Until recently, border security and immigration control were seen as two of the best frontline defenses against not just terrorism, but also threats to global health security such as infectious disease. But in today’s global village, where the scale and speed of human migration is unprecedented in all directions, deadly pathogens know no boundaries.
Until recently, border security and immigration control were seen as two of the best frontline defenses against not just terrorism, but also threats to global health security such as infectious disease. But in today’s global village, where the scale and speed of human migration is unprecedented in all directions, deadly pathogens know no boundaries.
Ultimately, if we want to keep the bugs at bay, we need to stop focusing all our attention on defending borders and instead look at how we can prevent outbreaks in the first place.
To understand how diseases can still pose a threat globally, consider measles, one of the most infectious diseases known to humanity – orders of magnitude more so than Ebola. It is possible to catch measles off someone just by entering the same room, even hours after they have left. Because of this, measles has become, in global health security terms, the proverbial canary in the coalmine.
Whenever and wherever measles outbreaks occur, it tells us something is not working. Whether it’s in Liberia where devastating health systems have left children unvaccinated and vulnerable, or in Disneyland, California, where measles is only rarely fatal yet one-in-eight children are now nevertheless at risk; a measles outbreak is an indication of an underlying problem.
That’s because measles is so infectious it requires an extremely high level of immunization coverage to achieve widespread protection within a community – so-called herd immunity. For many common infectious diseases, around 80% to 85% of the population need to be immunized to prevent their spread.
But with measles, if vaccination coverage drops below 90% it is just a matter of time before an outbreak occurs. So effectively measles raises the bar in terms of the level of immunization required to ensure prevention.
There are a number of reasons why we might fall short of this mark, and why we see outbreaks all over the world. For example, in Sudan the cause is primarily a lack of access of humanitarian aid to people trapped in conflict zones, while in California it is because of anti-vaccine groups whipping-up unfounded fears about the safety of vaccines.
But while any outbreak, no matter how small, is capable of spreading the virus – as we saw just a few years ago when outbreaks in South America were triggered by cases exported from Europe – it is the wider communities with consistently low immunization coverage that help to perpetuate the existence of the virus.
That is why it is mainly in the very poorest and most vulnerable communities where we see the largest outbreaks, places where it is that much harder to ensure that all the pieces are in place to achieve and maintain high levels of immunization coverage.
And that is where we need to concentrate our attention if we want to prevent future outbreaks and make the world safer from infectious disease. Because the parts of the world that are missing out on measles vaccinations and routine immunization are also most likely missing out on other vital health interventions.
It is time for a new approach.
Addressing this is partly about improving health systems, which play a vital role in increasing universal health coverage, boosting access to health interventions and building resilience against public health threats, both in terms of logistics and by simply making people physically less vulnerable.
But this alone won’t stop epidemics. For that countries also need better surveillance for rapid detection of public health threats, they need response plans, personnel who are trained to recognize threats and in-country laboratories that are capable of identifying diseases quickly.
The recent Ebola epidemic in West Africa provided clear evidence of this. The collapse of weak health systems may well have helped to exacerbate the outbreak, but it wasn’t a lack of shiny new hospitals that allowed things to get out of control. Rather, it was the fact that it took nearly three months before a laboratory diagnosis could be confirmed, coupled with a lack of preparedness and the absence of a suitable response strategy.
So while it is true that a lack of health provision and vital public health services makes it tougher for poor countries to cope with epidemics, it is also true that the absence of these facilities and services creates conditions that are ripe for epidemics to occur in the first place.
By failing to address this reality we are effectively increasing the global health security threat.
Ultimately what is needed is a radical shift in perspective; if we are to be successful in making the world safe and secure from the threat of pathogens, then we need to stop thinking of the spread of infectious disease as an invading force and instead see it for what it really is – a need for universal prevention.
By Dr. Seth Berkley, CEO of Gavi, the Vaccine Alliance – Gavi is an international organization created to improve access to new and underused vaccines for children living in the world’s poorest countries.
Source: Fox News