Leading experts from academia, industry and the public sector came together to share insights into novel diagnostics for infectious diseases.
Over two days in March, 40 international speakers and over 200 in-person and online attendees explored novel diagnostics technologies and what it takes to translate them into tools for the detection, pathogen identification and treatment of infections.
Professor Mike Levin, Department of Infectious Disease, presented an overview of the need for improved diagnostics: when patients present with signs of an infection, current methods often take days to return a result, and infectious pathogens can easily be missed in a clinical sample. Despite huge efforts, specific pathogen identification fails in approximately 75% of hospitalised cases.
As a consequence, most treatment is given without even knowing whether an infection is bacterial or viral, let alone identifying the specific causative agent or whether it is resistant to different drugs. Although many cases are caused by viruses, the vast majority of patients receive antibiotics, which do not treat viral infections, leading to worse patient outcomes and the overuse of antibiotics. The failure to identify the pathogen is particularly serious for patients with sepsis, where early treatment with appropriate antibiotics is essential.
In addition to the need at the individual patient level, diagnostics are also critical for disease surveillance and for monitoring the risk of hospital-acquired infections. Diagnostics are also needed to combat antimicrobial resistance (AMR), which is largely driven by the overuse of antibiotics.
Low-resource settings have specific diagnostic needs, as exemplified by findings from a 2021 report by the African Development Bank Group, which showed that only 15% of the African population have access to diagnostic services.
A number of common themes emerged from the discussion over the two days.
What is needed to bring impact?
Developing a new diagnostic device needs far more than engineers creating a new technology or biologists identifying a novel biomarker. An integrated approach must be taken that considers the science, clinical need, and how it will be used in the real world. As noted by Dr Tim Rawson (Department of Infectious Disease and NIHR Health Protection Research Unit in Healthcare Associated Infections and Antimicrobial Resistance), the lack of focus on societal value is another current barrier to the adoption of novel diagnostics. Presenters, including Dr Peter Buckle (Department of Surgery & Cancer and NIHR London in vitro Diagnostics Cooperative) described several critical questions that must be answered in the development of a new diagnostic:
- What is the clinical need?
- What is required of the diagnostic device – for example a binary yes/no answer, or a detailed identification, quantification, or nucleotide sequence?
- Where will it be used – in a hospital, rural health care clinic, or at home?
- Who will be using it – trained microbiologists, clinicians, community workers?
- Can it be integrated into patient flow?Which patients should be tested?
Professor Aubrey Cunnington, Department of Infectious Disease, said that new diagnostic technologies should incorporate the REST-ASSURED criteria, which include being rapid, scalable, affordable, equipment-free, and user-friendly, with connectivity of results in real-time.
Fulfilling many of these requirements – and a common feature of all the technologies discussed – is the move to point-of-care (POC) testing, which can eliminate the need for specimen culture, can be run with little technical expertise, and provide results within minutes
New technologies
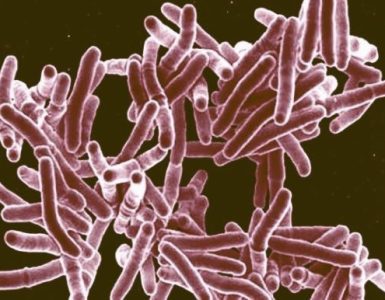
One such POC technology is ProtonDx, which was presented by co-founders Professor Pantelis Georgiou (Department of Department of Electrical and Electronic Engineering) and Dr Jesus Rodriguez-Manzano (Centre for Antimicrobial Optimisation). The technology is based on the release of protons during DNA and RNA amplification reactions, which can be measured colourimetrically (as used in ProtonDx’s DRAGONFLY platform) or electrochemically with lab-on-a-chip detection technology. The latter has been translated into LACEWING, a fully automated handheld, rapid and accurate molecular diagnostic platform. The systems are being tested for diagnosis of malaria, TB, dengue, SARS-CoV2, respiratory infections, new emerging infections, fungal infections, mPOX, HIV, and agricultural pathogens.
Describing another major diagnostic focus at Imperial, investigators from the international DIAMONDS consortium spoke about host biomarker-based diagnostics, analysing the patient’s immune response to provide a diagnosis or predict severity of disease. The strategy exploits the different patterns of gene and protein expression that are made in response to different pathogens. Such molecular profiles have been identified that can answer questions such as “Is the infection viral or bacterial?” or “Is the infection tuberculosis?”, which can be incorporated into simple diagnostic platforms. The team is also validating more complex signatures, incorporated in multiplex PCR platforms, that can determine whether the infection is one (or more) of eight conditions.
Closing the host-based biomarker talks, Dr David Antcliffe (Department of Surgery and Cancer) described the work of the GAinS consortium, which has defined distinct ‘sepsis response signatures’ that have the potential to predict outcome and inform treatment in critical care.
Imperial researchers are also improving lateral flow tests (LFTs). For example, Dr Leah Frenette (Department of Materials) described how nanoparticles with enzyme-like activity are being used to develop LFTs with very low detection limits. The technology is being tested for diagnosis of HIV, COVID-19, malaria, cholera, as well as non-communicable diseases. Finally, as shown by Professor Tony Cass (Department of Chemistry), highly sensitive LFTs are also being developed that use combinations of aptamers that can simultaneously detect a specific strain of virus (e.g. influenza virus) while eliminating contaminating subtypes.
Meeting the needs of low-resource settings
Point-of-care tests are particularly critical for low-resource settings. Speakers throughout the event described the barriers in such settings, which can include lack of access to healthcare settings, the absence of the Internet for notification of results, and expiry of test reagents. AMR was described as a significant problem, contributed to by the lack of diagnostics.
Addressing some of these barriers is the HIVQuant Project, presented by founder Dr Catherine Kibirige (Department of Infectious Diseases). The project is developing ambient-temperature HIV quantification kits that they hope will be used for early infant diagnosis and treatment monitoring, even at secondary or primary healthcare facilities in resource-constrained settings. This will be essential in curbing HIV drug resistance to readily available HIV treatments in LMICs. Use of room-temperature reagents is being explored alongside detailed consumer needs research.
Dr Florence Pradel also described the efforts and projects of Fondation Mérieux to promote capacity building, knowledge sharing, and antibiotic stewardship in low and middle income countries. A number of speakers presented innovations to combat tuberculosis (TB), both for initial diagnosis and resistance analysis. The recent addition to WHO policy recommendations for TB resistance diagnosis of culture-free targeted next-generation sequencing (NGS) was hailed as a significant move forward by Dr Andrea Cabibbe and was further highlighted by Dr Daniela Cirillo (Ospedale San Raffaele, Italy).
Assessing antibiotic susceptibility
The need for tools to determine whether a patient’s strain of pathogen is sensitive or resistant to an antibiotic, termed antibiotic susceptibility testing (AST), was a major theme of the workshop. A number of different platforms and detection strategies were showcased, including one that detects nanomotion, or microscopic movement of cells positioned on tiny ‘springboards’ (Resistell™, Dr Alex Sturm), another that is based on a microfluidic system (iFAST; Professor J Mark Sutton), and another that uses optical electrophysiology (Cytecom; Dr Magdalena Karlikowska).
It was emphasized, among others by Dr Christopher Longshaw (Shionogi), that when new antibiotics are developed, the associated susceptibility tests should be developed in parallel and incorporated into clinical trials. Dr Elita Jauneikaite, from the School of Public Health, showed how whole-genome sequencing is being used in AMR surveillance, including to monitor the spread of resistant strains.
Translation and adoption
Professor Graham Cooke (Department of Infectious Disease) described how translating ideas from academia into useful tests is a long and laborious process that involves discovery (e.g., of biomarkers, sensors, algorithms for classification models), translation (e.g., validation), and adoption. Dr Vjera Magdalenic-Moussavi (Imperial Enterprise) described the path from idea to spinout as well as the steps and funding options around intellectual property. A clear theme that emerged was the need for collaboration and convergence science. In academia, links across disciplines are crucial and must be complemented by collaboration between healthcare systems, academia, and industry. Developers must also work with users – clinicians, patients and public, decision-makers, and payers – early on in the development process to ensure alignment with real world needs and systems.
Many presenters – including Dr Annie Truong from the Medicines and Healthcare products Regulatory Agency (MHRA), Dr Anita Suresh from FIND, and Nishan Sunthares from the Association of British HealthTech Industries (ABHI) – described the complex regulatory and adoption landscape and the large amount of data and evidence (clinical, unmet need, quality, and economic) required by a range of regulators and policymakers, including government bodies, payers, health systems (e.g., the NHS) and the WHO. Even with regulatory approval and favourable clinical and cost-effectiveness evidence, there was consensus that adoption is not guaranteed: implementation may require consideration of additional aspects such as cultural factors, incentives, and education and infrastructure.
Resources are available to help with the translational and regulatory pipeline, including university Enterprise teams (for IP), NIHR London In vitro Diagnostics Cooperative (for patient and public involvement), FIND (for assembly of evidence for submission to WHO, especially for diagnostics targeting LMICs), and ABHI (for coordination with governments, NHS, and regulators).
Standardisation
The final theme that emerged was the essential need for standardisation of reagents, resources and protocols, to ensure comparability between assays, between laboratories and between countries.
There were calls for:
- Standardised bioassay methods and technologies, needed for the quantification of aspects such as antibiotic sensitivity and viral load
- Central biobanks, which can provide standardised isolates
- Platforms containing gold-standard test and validation data sets, which are needed to ensure that new markers and assays are truly interpretable, translatable, and generalisable to all populations in the real-world setting
- Databases of resistance determinants that define the minimum array of targets that should be incorporated into AST assays
- Standardised bioinformatics-based workflows for AMR gene detection using whole genome sequencing data, as illustrated by the BenchAMRking© platform presented by Dr John Hays, Dr Nikolaos Strepis and Dr Andrew Stubbs from the Erasmus University Medical Centre, Rotterdam (Erasmus MC).
Funder session and declaration
In the penultimate session of the event, moderated by Professor Till Bachmann (University of Edinburgh), representatives from five funders presented their priorities and upcoming opportunities for funding diagnostic research and development. The importance of defining the clinical need and collaboration was reiterated.
Finally, Dr Leonid Chindelevitch (School of Public Health), who also leads the B2B2B network on AMR diagnostics, presented and led a discussion of the document “Declaration: Infectious disease and antimicrobial resistance diagnostics, an urgent need for global health.” The declaration, already endorsed by dozens of signatories, will call on governments globally to invest and take more action to reduce the barriers facing novel diagnostics in order to impact global health.
The event was co-organised and funded by Imperial College London’s Institute of Infection, JPIAMR-funded B2B2B Network, London In Vitro Diagnostics Co-operative, NIHR Imperial Biomedical Research Centre, and DIAMONDS consortium, with further funding provided by a UKRI Impact Accelerator Award for Healthy Society and the Rosetrees Trust.
Source: Imperial College London