 On any given day, one out of 25 patients in a U.S. hospital has at least one hospital-acquired infection, and Clostridium difficile infection (CDI) is the most common.
On any given day, one out of 25 patients in a U.S. hospital has at least one hospital-acquired infection, and Clostridium difficile infection (CDI) is the most common.
CDI is regarded as one of the serious, expensive, and potentially avoidable consequences of hospitalization. The length of stay can extend to 21.3 days, with estimated costs of up to $29,000 per episode of hospital-acquired CDI. The excess costs to U.S. acute-care facilities are estimated to be $4.8 billion.
According to the Centers for Disease Control and Prevention, there are nearly half a million CDI cases in the U.S. each year and CDI is the leading cause of gastroenteritis-associated death; nearly 30,000 patients died within 30 days of diagnosis.
As rates of CDI increase, so does the pressure on physicians, clinical laboratories, and hospital administrators to reduce outbreaks and contain the costs. Institutions may be fined thousands of dollars for each incidence of CDI.
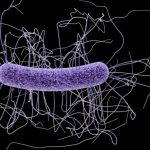
Clostridium difficile
C. difficile (now reclassified as Clostridioides difficile) is a spore-forming bacterium found in air, water, soil, and feces. It can colonize in the colon and begin producing toxins, often after use of antibiotics disrupting the normal flora. Symptoms associated with CDI include diarrhea, severe cramping, fever, nausea, and dehydration.
Challenges of diagnosing CDI
A significant challenge is in the laboratory diagnosis of CDI, as no single test can definitively identify CDI, and currently available methods are hampered by poor sensitivity, specificity, or long turnaround times. An incorrect result can lead to overdiagnosis and overtreatment or missed cases of infection. To compensate for these inadequacies, guidelines released earlier this year by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America recommend multistep testing algorithms involving two or more detection methods, unless patients with high pretest probability are tested, something that is difficult both to define and implement.
Identifying CDI is complicated and uncertain from the start. The process begins with a complex series of questions, such as:
- Is testing appropriate? Has the patient had three or more incidents of loose stools in the last 24 h that were unformed, unexplained, and recurring?
- Was there recent laxative use?
- Is the patient symptomatic?
- What about recent antibiotic use?
Often, patients with suspected CDI are isolated prior to testing. Isolation can be stressful to patients, costly to hospital bed management, and add to the burden to hospital staff.
Once the questions are answered and an appropriate specimen is collected, laboratory testing methods currently available offer varying levels of certainty.
- Nucleic acid amplification tests (NAATs) offer high sensitivity and can identify whether a toxigenic C. difficile organism is present in a patient’s stool, but not whether it is producing disease-causing toxins. This lack of clinical specificity makes molecular testing susceptible to false positives.
- Traditional Immunoassay tests are specific enough to detect the actual toxins that cause disease, but they lack sufficient sensitivity making them susceptible to false negative results.
- Use of cell cytotoxicity neutralization assay, the gold standard for toxin detection, offers high sensitivity and specificity but is labor-intensive, operator dependent, and takes time (24-48 hours).
Uncertainty leaves clinicians concerned about the consequences of overtreating or undertreating patients. Patients treated unnecessarily with antibiotics are at increased risk for true CDI. Risks to patients with CDI left untreated can be significant; patients get increasingly ill, the infection may spread within the hospital and to otherwise healthy family members. Identifying and appropriately treating this infection is critical and, often, life-saving.
The future of C. difficile testing is close
A simple, rapid, and cost-effective solution that offers high sensitivity and high specificity in one test is in development, to address current challenges and potentially change the way CDI is diagnosed.
Findings from studies presented at the European Congress of Clinical Microbiology and Infectious Diseases and at the American Society for Microbiology demonstrate a new C. difficile toxins A/B assay offering a single-test solution with both high sensitivity and high specificity. The new test detects toxins at 100 times lower concentrations than current immunoassays and delivers clinically actionable results in less than 35 minutes
One study conducted by Dr. Niaz Banaei of Stanford University Medical Center, demonstrated that a C. diff toxins A/B assay in development by Singulex (for investigational use only) yielded 98% sensitivity and 100% specificity compared to a multistep PCR-and-toxin testing algorithm.
A second study showed this C. diff toxins A/B assay demonstrated reactivity to common C. difficile strains, did not show cross-reactivity to common gastrointestinal pathogens, was robust against common interferents at relevant concentrations, allowed for detection of toxins in both fresh and frozen stool samples and up to three freeze-thaw cycles, and provided results with high reproducibility9.
The test runs on a platform powered by Single Molecule Counting technology, a novel immunoassay technology recognized for its unprecedented sensitivity and precision in the measurement of biomarkers.
A single-step C. difficile diagnostic solution enables the lab to address a critical need.
So far in 2018, 751 hospitals have been penalized for rates of hospital-acquired conditions10. Control of these infections, including prevention and management of CDI, is a priority.
The availability of a single-test solution for the rapid detection of CDI could play a significant role enabling the laboratory, clinicians, and hospital administrators to address a growing problem with wide-ranging ramifications. Improved accuracy and confidence in diagnosis will contribute to improved antibiotic stewardship, and decrease costs associated with incorrect isolation and increased length of stay.

















