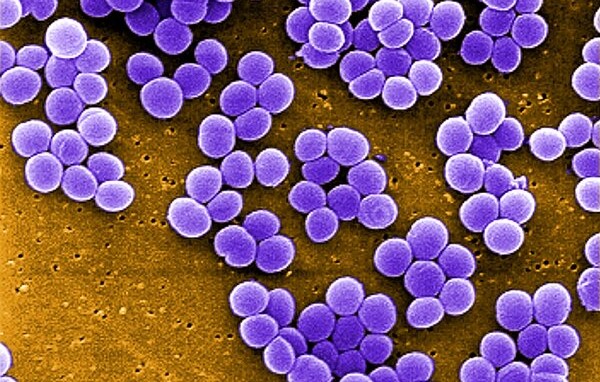
In the spring of 2011, pharmaceutical giant Merck and its collaborators learned that a data monitoring committee was calling for a halt of their phase 3 clinical trial. The vaccine candidate they had built against Staphylococcus aureus—the leading cause of death by bacterial infection worldwide—and had tested among 8000 patients across 26 countries wasn’t effective enough to move forward.
“That was the start of it, but that wasn’t the end of it,” said Vance Fowler, MD, MHS, an infectious disease specialist at Duke Health and a lead investigator for the trial.
A deeper look at the data over the following year brought troubling news for the shuttered study, which had tested the vaccine candidate in patients undergoing cardiothoracic surgery. Participants in the trial who developed an S aureus infection were more likely to die if they had received the vaccine than if they had gotten the placebo shot. Many of the vaccine recipients who died did so with multiorgan system failure, Fowler noted, and experts speculate that the risk may have arisen in part from an amplified inflammatory response. But researchers still aren’t certain how the investigational vaccine made recipients more vulnerable.
“It’s not what any of us were expecting,” Fowler said.
In 2012, while the vaccine world was still reeling from the damage of the Merck trial, Pfizer launched its own trial of a candidate that included 4 different S aureus antigens. Based on promising efficacy data in mice, Pfizer tested it first among healthy adults and then in more than 3000 patients undergoing elective surgeries. But by 2018, hope for this vaccine too had dissipated. Serum data showed that although patients who had received it developed antibodies to S aureus, they contracted the infection at the same rate as the placebo group. Like Merck’s study before it, the phase 2b trial was discontinued.
Passive immunization with monoclonal antibodies, which are infused to provide short-term protection, has also failed to prevent or treat S aureus infections. Two monoclonal antibodies in development—Arsanis’ ASN100 and Aridis’ suvratoxumab—did not prevent ventilator-associated pneumonia in midphase trials in 2018 and 2021, respectively. And just last year, Aridis’ monoclonal antibody candidate tosatoxumab did not meet its primary efficacy end point for treating S aureus ventilator–associated pneumonia in a phase 3 study.
In fact, over the last quarter of a century, approximately 14 investigational S aureus vaccines have failed in phase 2 or 3 clinical trials. One vaccine developer after another poured millions of dollars into a candidate backed by elegant science. But no matter how promising the strategy or how well the candidate worked in preclinical studies, not one of them has successfully protected humans from S aureus.
After the Merck trial, the string of unexplained vaccine failures became “an elephant in the room,” said George Liu, MD, PhD, division chief of pediatric infectious diseases at the University of California, San Diego, where his laboratory studies S aureus.
“We realized what we needed is something that could explain not just one vaccine, but lots of vaccines, not working,” he said.
The problem, it turns out, is a limited understanding of the foe. Research from Liu’s laboratory shows that S aureus doesn’t interact with the immune system like other microbes for which there are effective vaccines. The pathogen has a means of manipulating the immune system for its own protection, rendering host defenses and classic vaccine strategies nonprotective. It’s an explanation for the years of failed trials. And it’s offering hope for a vaccine that might work.
Model behavior
S aureus, the most common cause of staph infections, walks a thin line between innocuous neighbor and threat. It’s what scientists call a pathobiont—a pathogen that lives with humans without causing harm most of the time. As many as a third of adults and 50% of children persistently carry it in their nose with no symptoms and another 60% carry it intermittently. A majority of infants are colonized in the first 6 months to 1 year of life. And for the most part, S aureus remains a harmless member of the skin, nose, and gastrointestinal microbiota.
But given the chance to cross into the blood, lung, or soft tissue, S aureus can become lethal. Medical devices, surgical procedures, uncovered wounds, and injection drug use are all common ways people contract S aureus infections, which can lead to sepsis, pneumonia, endocarditis, and bone infections. Staph infections are responsible for more than 1 million global deaths and billions of dollars in US hospitalization costs annually. And the microbe’s increasing resistance to antibiotics is also limiting treatment options, upping the urgency for a vaccine.
As the failed vaccine trials continued to mount, Liu began to look into the one factor almost all the trials had in common: the animal model. Behind nearly every failed human S aureus vaccine trial was a successful preclinical study in mice. If the protective benefits never carried over to humans, clearly the mouse model wasn’t a good predictor for human immunity, Liu explained. Something was fundamentally different about the mouse model and humans.
The most obvious difference to Liu was that people live with S aureus and laboratory mice don’t.
So he ran an experiment.
His team preinfected mice with S aureus in the weeks before they received a vaccine similar to the one used in the Merck trial to see if the exposure had any effect on their subsequent response to the vaccine. In the control mice that had never been exposed to S aureus, the vaccine “worked beautifully,” Liu said. But in the mice preexposed to S aureus, the vaccine wasn’t protective.
The results, reported in the journal Cell Host & Microbe in 2022, mirrored what researchers had seen in clinical trials: when S aureus reaches an immune system first, something goes awry and vaccines don’t work.
Memory problems
A closer look at their antibodies showed that S aureus was perturbing the rodents’ immunological memory.
The immune system builds antibodies in response to foreign molecules called antigens. After encountering an antigen once, the adaptive arm of the immune system commits the matching antibody to memory. If the pathogen is met again, those antibodies can be quickly recalled. This immunologic memory is crucial for long-term protection.
But S aureus had learned to hack it.
Liu’s study showed that when laboratory mice are exposed to S aureus, the pathogen imprints a faulty immune response. The immune system learns to build anti–S aureus antibodies that rush to the scene but can’t generate protection.
Normally, an antibody would bind to an antigen on the bacterium’s cell wall and then drag the microbe to a macrophage or neutrophil-immune cell to be digested and destroyed in a process called phagocytosis. But in Liu’s study, mice that were exposed to S aureus produced antibodies that carried an extra sugar group. These antibodies still attached to the bacterium’s surface, but when they reached macrophages, the immune cells didn’t destroy the pathogen. When the researchers removed the sugar group, phagocytosis was restored.
This immune manipulation allows S aureus to live commensally with humans, but it also undermines vaccination. When a mouse or a person who was already exposed to the bacteria is vaccinated against it, their immune system preferentially recalls the original immune response instead of building a new protective one based on the vaccine.
“Because of the nature of immunologic memory, the body will simply amplify that [initial] response,” said Juliane Bubeck-Wardenburg, MD, PhD, division director of pediatric critical care medicine at Washington University School of Medicine in St Louis, who studies S aureus pathogen-host interaction. “It’s very difficult to rewire an existing immune response once it’s already established on a trajectory that is unfavorable.”
In a follow-up study published late last year in Cell Reports Medicine, Liu’s group broadened their research to look at 10 S aureus antigens, many of which had failed in clinical trials. These included 8 active vaccine antigens, which prompt the body to build its own antibodies, and 2 monoclonal antibody candidates, suvratoxumab and tefibazumab.
Active vaccine antigens associated with S aureus’ cell wall offered no protection in mice that were previously exposed to the microbe. These vaccines recalled and intensified the nonprotective immune imprint.
The monoclonal antibodies were also ineffective in S aureus–exposed mice, but for different reasons. They couldn’t compete with the nonprotective endogenous antibodies preprogrammed by S aureus. These endogenous antibodies were bound to the bacterial cells, so when the monoclonal antibodies arrived, they had nowhere to latch on. Normally endogenous antibodies “would pounce and kill pathogens,” Liu said. “Instead, endogenous staph antibodies come in and protect the bacteria from being killed by the therapeutics.”
A new work-around
Although most of the antigens examined in Liu’s 2023 study fell to S aureus’ immune evasion techniques, the work suggests there’s still room for optimism.
One of the active vaccine antigens induced neutralizing antibodies against a key S aureus virulence factor called α toxin—even in previously exposed mice.
“Bacterial toxins give bacteria an advantage over host immune response,” Bubeck-Wardenburg said. “Neutralizing them resets the balance and gives the immune system more window of opportunity to fight the infection.”
The study also showed some promise in targeting so-called subdominant antigens. A pathogen like S aureus has multiple antigens, and some elicit a bigger immune response than others. The bacteria’s dominant antigen, iron-regulated surface determinant B, or IsdB, induces the nonprotective antibodies. Liu’s team found it more effective to target subdominant antigenic regions that elicit a smaller immune response but may not be protected by faulty immune imprinting.
Research outside the Liu laboratory also points to the importance of T cells for thwarting S aureus. A 2014 follow-up analysis of a subset of patients from the Merck clinical trial found that mortality was strongly associated with low levels of certain T-cell cytokines in the vaccine recipients’ serum. The study was small and hypothesis-generating, but “the takeaway is that the patients who died seemed to have inappropriate or nonexistent T-cell responses to vaccination despite having plenty of antibody,” Chris Montgomery, MD, a critical care physician at Nationwide Children’s Hospital, wrote in an email.
Data from Bubeck-Wardenburg and Montgomery’s laboratories suggest the S aureus α toxin impairs T-cell development and deters vaccine response. Patients with T-cell dysfunction also show higher vulnerability to recurrent S aureus infection, which may indicate that these immune cells play a critical defense role, Bubeck-Wardenburg said.
Ultimately, the best approach for future vaccines will likely be multivalent, Duke University’s Fowler said. These vaccines will target some combination of toxins, T cells, and multiple other antigens from different phases of the S aureus life cycle and stages of infection.
There’s also the question of who should be vaccinated. To date, vaccine developers have focused on patients already colonized with S aureus and at high risk of infection. But some experts say vaccinating infants is the better strategy. “Our childhood vaccination infrastructure is amazing,” said Montgomery, whose research focuses on S aureus pathogenesis. Vaccinating infants could allow the immunization to take effect before S aureus fully imprints the immune system, he noted.
Before jumping into new vaccine strategies, experts agree that the field needs a better understanding of how the human immune system interacts with S aureus. We have to “accept we may not know as much about S aureus immunity as we thought we did,” Fowler said.
“If we don’t know what is truly protective in humans then everything that we are doing in preclinical models is just guessing—informed guessing but guessing nonetheless,” Montgomery added.
This is the work Liu is doing now. His team is investigating the fundamental mechanism underlying why the imprinted immune response is not protective. If researchers can figure this out, he wonders if they may actually be able to reverse it. Perhaps, he suggests, they can sidestep the need for a new vaccine altogether and simply “convert the nonprotective memory into a protective memory.”
Source: JAMA Medical News