 New technologies give vaccine developers a boost in early development, but large-scale testing and production are bogged down by high costs and lengthy trials.
New technologies give vaccine developers a boost in early development, but large-scale testing and production are bogged down by high costs and lengthy trials.
Middle East respiratory syndrome, or MERS, is spreading across the globe, and while a vaccine could be developed, there’s little commercial incentive to make one.
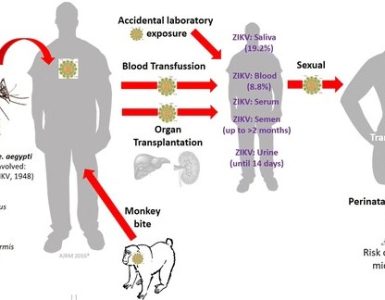
The deadly virus was first identified in Saudi Arabia in 2012. Since then, infected people have turned up in Europe, Africa, and Asia. The first cases arrived in the United States this month, beginning with two infected travelers returning from Saudi Arabia. On Saturday, authorities reported the first person-to-person transmission within the U.S., most likely from a face-to-face conversation.
While DNA sequencing and synthesis and other biomedical technologies offer ways to quickly devise experimental treatments for sudden disease outbreaks like MERS, the greater challenge is the formidable cost and time needed to test a new vaccine.
The need for a MERS vaccine certainly seems urgent. While the U.S. resident most recently reported to have been infected by MERS is said to have recovered with no medical intervention, he is believed to have been infected from a face-to-face business meeting that lasted just 40 minutes. Others have not had such fortunate outcomes.
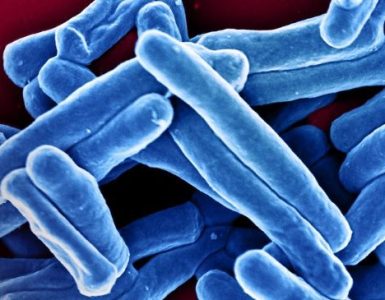
Approximately one-third of those diagnosed with MERS have died, according to the Centers for Disease Control and Prevention. The virus is transmitted from person to person—including from patient to health-care worker—and symptoms include fever, cough, and shortness of breath.
Unfortunately, drug companies see less urgency. And while researchers can develop experimental vaccines quickly enough, it typically takes a big pharmaceutical company to test and manufacture it. There just aren’t enough cases of MERS yet to establish a guaranteed market for a vaccine.
“In the U.S., generally speaking, it will take a decade or more and just shy of a billion dollars to get a vaccine licensed through the FDA,” says Gregory Poland, who heads the Vaccine Research Group at the Mayo Clinic. The reason is human testing, which is costly and must prove not only that a vaccine works but also that it produces no harmful side effects.
Furthermore, because viruses can mutate quickly, the financial risks can be huge, says William Carter, CEO of Hemispherx Biopharma, a Philadelphia-based company developing treatments for viral infections including MERS. “The apparent utility of the vaccine can vaporize before your very eyes,” he says.
New technologies do allow experimental vaccines to be developed quickly, although those vaccines still require testing. In March 2013, the first cases of people being infected by the avian flu H7N9 were identified in China. Ten days after the Chinese government announced the outbreak, the biopharmaceutical company Novavax—which was already working under a contract with the U.S. government to develop a vaccine against the H5N1 bird flu—received the genetic sequence of the virus and began developing a vaccine. Just six months after the H7N9 virus was sequenced, Novavax’s experimental vaccine was tested in humans with positive results. The company continues to develop the product with U.S. government support, although it must still go through lengthy testing.
The approach used by Novavax shows how rapidly a vaccine can emerge from the lab bench. Instead of copying viral DNA using bacteria, which requires acquiring a copy of the virus’s genome, a potentially time-consuming process, the company had the DNA synthesized chemically, then used cultured insect cells to produce bits of protein from that DNA. The protein bits were combined into a virus-sized nanoparticle that was used as the vaccine.
Despite a lack of market incentives for now, a few companies are trying to develop vaccines against MERS. Among them are Novavax, which is using the same methods employed for its H7N9 vaccine. But these companies face a unique technical challenge: for some unknown reason, no small lab animals can be infected by MERS.
And so, while researchers at the University of Maryland School of Medicine reported last month that Novavax’s vaccine can generate anti-MERS antibodies in mice, they could not show whether that immune response actually protected the animals against any disease. The next step will be finding a suitable animal for testing, perhaps a non-human primate or a mouse that has been genetically altered to be susceptible.
Source: MIT Technology Review