 Proteins never get to where they need to be to start an antiviral attack.
Proteins never get to where they need to be to start an antiviral attack.
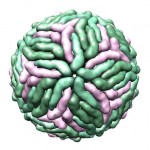
The Dengue virus comes in four distinct but related varieties called serotypes, and they’re all bad. Rather than inducing tolerance for each other, infection with one Dengue serotype actually makes people more sensitive to the other three. Victims infected by a second serotype can develop hemorrhagic fevers, which can be fatal. Somewhere around 400 million people are infected with Dengue annually—more than any other mosquito-borne ailment. There is no cure.
Dengue is also in the same family as Zika and is spread by the same mosquitos, so learning more about one could have broad applications for the other. Researchers published a paper in Nature describing how the Dengue virus avoids one arm of our immune system.
There are two arms to our immune system. Adaptive immunity generates antibodies and T cell receptors to combat unique aspects of a specific pathogen. After the fight is over, these antibodies and receptors stick around to remember and attack that pathogen should we encounter it again. Antibodies and T cell receptors form the molecular premise upon which vaccines are based.
The other arm is innate immunity, a more primal system in which our immune cells recognize generic features that indicate “invader!” Dengue can evade both and replicate nearly unchecked in our cells. Recent work has just revealed one way in which Dengue skirts our innate immune system, which may hopefully pave the way for antiviral therapies.
When a virus like Dengue infects us, pathogen-sensing proteins in our immune cells recognize it as foreign and threatening because of its nucleic acids (Dengue has RNA, rather than DNA). At this point, these proteins rush from their stations throughout the cell and gather on the outer mitochondrial membrane. From here, they elicit the expression of signaling molecules called interferons and inflammatory cytokines. Interferons and cytokines drive cells to clear the infection and activate the adaptive immune system.
But Dengue has proteins of its own. One of them, NS3, is known to antagonize interferons, but until recently we didn’t know how. Now, Nature describes how, even though we have a protein in our immune cells that recognizes Dengue’s genomic material as foreign, that protein can’t accomplish anything useful.
That’s because the protein that recognizes Dengue needs a molecular escort—also called a trafficking protein—to move it to the surface of the mitochondria where it can be useful. Dengue’s NS3 binds to and lures that escort away from the recognition protein. All four serotypes of Dengue share the region of NS3 that binds to the escort, as does West Nile virus. (Viruses like hepatitis C and yellow fever, although related to Dengue, lack this ability.)
When the researchers mutated this region of the NS3 protein, they eliminated its ability to interact with molecular escorts. Viral replication was significantly reduced, interferons got switched on, and the innate immune system was generally more active.
This is the first indication that viruses target the molecular escorts that move things around in a cell. Since a Dengue virus that doesn’t impede this trafficking doesn’t mount an effective infection, perhaps it can act as a live attenuated vaccine.
Alternatively, small molecules might be designed to block the interaction between NS3 and the molecular escort to which it binds. This way the protein that sounds the alarm about a harmful microbe will get to where it needs to be to begin antiviral action.
Source: ars technica

















