In order for the Ebola virus (EBOV) to hijack a cell, it must first “board” its intended mass replication vehicle. The biomechanics of this process have been elusive, hindering the development of potential clinical therapies to treat the disease, as well as, control the spread of infection. Yet now, scientists from Lehigh University and the University of Iowa have developed a simple model for EBOV-host interaction. Findings from the new study were published recently in Scientific Reports through an article titled “Biomechanical characterization of TIM protein-mediated Ebola virus-host cell adhesion.”
It was recently reported that the number of Ebola cases in the Democratic Republic of Congo has surpassed 1,000, making it the second-worst outbreak in history after the 2014 outbreak in West Africa in which 29,000 people were infected and more than 11,000 died. This latest milestone is a stark reminder of the urgent need to develop effective prevention and treatment agents for this frequently deadly disease.
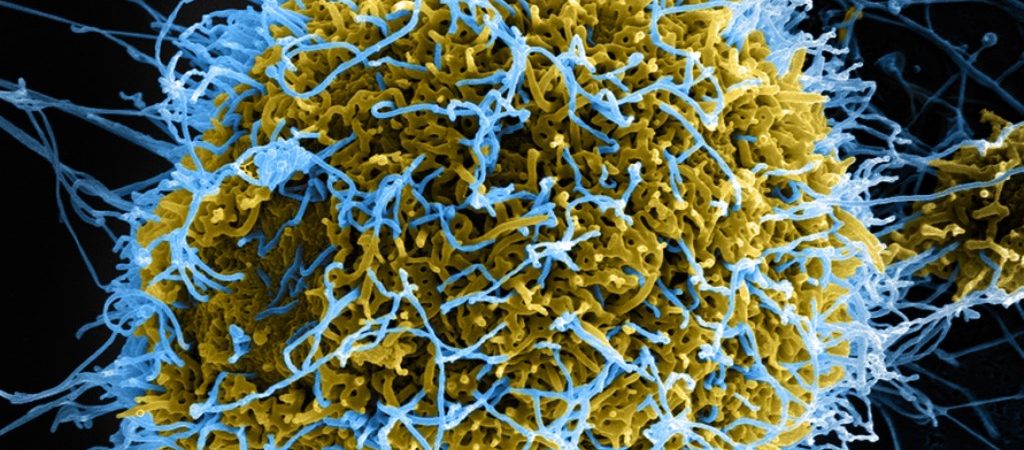
Key to developing treatments for the disease is understanding the mechanisms of the infection process. Scientists know that to enter a human cell, Ebola takes advantage of a natural process called macropinocytosis, through which the cell “cleans up” its surroundings by internalizing the dead cell debris that surrounds it. Proteins on a cell’s surface serve as receptors, allowing immune cells to recognize the dead cell debris and internalize it. The virus interacts with these proteins, called T-cell immunoglobulin and mucin domain (TIM) proteins and uses them to hijack its way into the cell. Once inside, the Ebola virus membrane fuses to the endosome that has formed around it and releases its genetic content into the cell.
“Viral RNA further hijacks the cell machinery to make proteins and replicate themselves inside,” explained lead study investigator Frank Zhang, PhD, associate professor of bioengineering and of mechanical engineering at Lehigh University “Then they bud off the membrane to form a new virus while the healthy host cell dies.”
“While Ebola-host cell attachment has been shown to depend on the molecular biomechanics of interaction between receptors on the cell surface and the outer coat of the virus, the quantitative understanding essential for guiding the development of therapies has yet to be developed,” added study co-author Anand Jagota, PhD, founding chair of the Lehigh’s department of bioengineering and professor of chemical and biomolecular engineering.
The researchers looked to better understand the biomechanics of Ebola virus-host cell adhesion. The project paired Jagota’s expertise in computational molecular adhesion mechanics with Zhang’s focus in mechanosensing, or how cells sense and respond to mechanical stimuli. The duo, working alongside colleagues from the University of Iowa, has developed a simple model that characterizes the biomechanics of Ebola virus-host cell adhesion findings that could provide new and helpful information on the road to developing an effective Ebola treatment.
“We utilized single-molecule force spectroscopy to quantify the specific interaction forces between the TIM proteins of a host cell and Ebola-virus-like particles,” Zhang noted.
In addition to illuminating the biomechanical parameters important for Ebola attachment to a host cell, the team also demonstrated experimentally that TIM-Ebola virus interactions are mechanically comparable to adhesion molecule (e.g., selectin) ligand interactions. Through a simple mechanical model, they further demonstrate how molecular binding parameters determine whether they are sufficient for viral adhesion.
The purpose of the model was to show how single-molecule measurements can be combined with other physical properties of the system, such as density of ligand-receptor pairs and membrane stiffness, to predict whether and to what extent a viral particle will adhere to the cell membrane. The team modeled attachment as being driven by adhesion between TIM proteins and phosphatidylserine on the surface of the virus (believed to mediate the virus-host cell attachment) and resisted by membrane bending.
“The model’s simplicity has allowed us to highlight the importance of two dimensionless groups of parameters and their potential ability to block adhesion,” said Jagota.
The researchers used single-molecule force spectroscopy to monitor, manipulate, and measure mechanical forces. For example, in the study, Zhang would bring a virus-like particle to a cell with its TIM receptor expressed, observe their interaction, and pull them apart to determine the mechanical strength of the interaction, or how much force is required to pull them apart.
Jagota than used mathematical models to understand the interaction between Ebola and the cell, what properties represent the Ebola virus—its stiffness, its shape—and what properties represent the cell—the components it presents on its surface—in this interaction.
“The hope is that this quantitative knowledge about the biomechanics of adhesion can be used to predict conditions for Ebola’s attachment,” Jagota concluded. “Long-term, the goal is for this information to help bring about new pharmacological targets and aid in the development of much-needed antiviral therapeutics for the prevention and treatment of Ebola.”