Non-neuroinvasive herpes simplex virus variant could be a highly regarded vaccine candidate
Non-neuroinvasive herpes simplex virus variant could be a highly regarded vaccine candidate
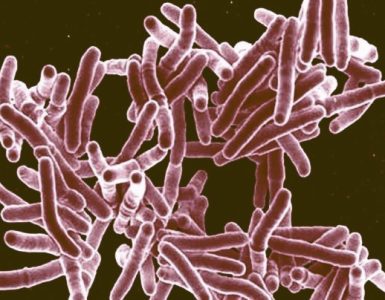
The worldwide need for an effective herpes simplex virus (HSV) vaccine remains a priority because it is a common infection that causes physical and economic disadvantages.
A new study published by Nature on November 6, 2020, reported the recent ‘failure of the subunit gD2 vaccine in a clinical trial demonstrated that new approaches to HSV vaccines are needed, especially those that present multiple HSV antigens.’
‘R2 is an attractive candidate because it is specifically ablated for retrograde axonal transport and therefore fails to invade the peripheral and central nervous systems, as initially demonstrated in mice and validated here in guinea pigs.’
‘The potential utility of a non-neuroinvasive HSV variant as a vaccine is highly regarded. However, early mutant viruses that were attenuated for neurotropism generally had broader replication defects in vivo that limited antigen presentation.’
Nebraska’s Gary Pickard and Patricia Sollars, alongside Northwestern’s Gregory Smith and Tufts University’s Ekaterina Heldwein, have spent years studying how to prevent HSV from reaching the safety of the nervous system, stated a University of Nebraska press release issued on November 6, 2020.
“You can keep the virus from getting into the nervous system,” said Pickard, professor of veterinary medicine and biomedical sciences at Nebraska. “But when you knock down the virus so much that it doesn’t replicate well, you are not rewarded with a robust immune response that can protect you from future exposures.”
Excerpts from this new study are inserted below:
The R2 design offers another solution to the challenge of producing a virus that replicates in the periphery inducing a strong immune response without seeding the nervous system and establishing a latent infection.
Instead of adjusting tissue tropism, R2 selectively eliminates retrograde axonal transport, which is fundamental to neuroinvasion. The design leaves all viral antigens intact for enhanced vaccine efficacy.
Thus, selective elimination of retrograde delivery to the nervous system is an attractive approach for the development of HSV vaccines, because it decreases concerns that a live-attenuated HSV vaccine could become latent, possibly revert or recombine, or subsequently cause complications if the immune system becomes compromised or distressed.
Similarly, the concerns that a persistent HSV vaccine virus could contribute to neurodegenerative diseases, such as Alzheimer’s disease, are eliminated.
The R2 vaccine encodes a mutated UL37 gene which contains three evolutionarily conserved surface-exposed regions: R1, R2, and R3.
Mutation of R2 produces viruses that propagate normally at peripheral sites of inoculation but fail to invade the nervous system by retrograde axonal transport, cannot establish a latent infection, and are avirulent.
The ability to selectively eliminate the neuroinvasive property of these viruses, without otherwise impairing their replication and thus the induction of immunity, provides an intriguing immunization paradigm.
The initial use of an HSV-1 R2 vaccine reflects the importance of HSV-1 in genital HSV infections and the importance of cross-protection, as both HSV-1 and HSV-2 are important human pathogens.
Evidence for cross-protection can be found in many animal experiments. In the recent clinical trial, a gD2 vaccine was more protective against HSV-1 than HSV-2.
Nevertheless, an R2 derivative of HSV-2 will be produced to determine if vaccine efficacy is further enhanced.
In the experiments reported here, we first evaluated the attenuation of the R2 vaccine following vaginal inoculation of guinea pigs, reasoning that this is a sensitive and well-described model of HSV pathogenesis. Interestingly, although the parent F strain was attenuated relative to HSV-1 strain 17syn+ in guinea pigs as we have noted previously, the R2 derivative was further attenuated, non-neuroinvasive, and avirulent.
Thus, R2 was also not detected in the DRG either early during infection or at day 28, times when the parent F strain and wild-type strain 17 syn+ were readily detected.
We next evaluated the protection afforded by the R2 vaccine against vaginal HSV-2 challenge.
R2 was administered by three routes (IM, ID, and IVag) and its efficacy was compared to a gD2+MPL/Alum vaccine, similar to the one used in the clinical trial. This comparison was intended to determine if R2 was at least as effective as the subunit vaccine and if R2 was more effective in the important outcomes regarding recurrent disease and recurrent virus shedding.
Therefore, we used the guinea pig genital model because it uniquely allows for the evaluation of these critical endpoints. The advantages of this model are more fully discussed in a recent review.
Protection was detected by R2 immunization using all 3 routes of vaccination but the ID route was consistently the most effective. Importantly, ID administration of the R2 vaccine-induced higher levels of neutralizing antibodies and provided greater protection than the gD2 subunit vaccine by several parameters.
Perhaps, this was due to the improved neutralizing antibody response and/or the ability of live-attenuated virus vaccines to induce T cell-mediated immunity that exceeds that of subunit vaccines.
In the experiments reported here, R2 vaccination by the ID route protected the most animals from acute disease and had the largest decrease in acute virus replication. R2 vaccination also decreased latent virus detection in the DRG as well as recurrent disease and recurrent shedding.
In comparison, the gD2 MPL/alum vaccine did not significantly decrease the number of animals with acute disease, acute vaginal virus titers, or recurrent vaginal virus shedding. Only further clinical evaluations of vaccines that have been evaluated in this guinea pig model will allow a better understanding of predictability.
There are several anomalies that should be pointed out in our data. The most important is the discrepancy between the number of animals with latent virus detected in the DRG and recurrent shedding. While we cannot currently reconcile these findings, one possible explanation is that gD2 MPL/Alum failed to protect against invasion and reactivation of HSV-2 from another latent site, perhaps autonomic neurons.
In summary, the live R2 HSV-1 vaccine is significantly attenuated in the guinea pig vaginal model and most importantly does not infect the nervous system within the limits of detection. R2 vaccination, especially by the ID route, provided protection against acute disease, recurrent disease, and recurrent virus shedding that was equal or superior to the gD2+MPL/Alum vaccine.
Given the encouraging findings with R2, a more detailed analysis of the correlates of protection is warranted and will be examined as part of future studies.
We consider these results highly encouraging, especially considering R2 is an HSV-1 virus and was evaluated for cross-protection against HSV-2 challenge.
Because no HSV vaccines have yet proven effective clinically, it is not clear what endpoints of the guinea pig vaginal model will predict protection in human evaluations, concluded these researchers.
These researchers did not disclose industry conflicts of interest.
Source: PrecisionVaccinations