Yves Hansmann and Aurélie Velay
E-CDC risk status: endemic
(data as of end 2022, updated May 2023)
History and current situation
The first human case of tick-borne encephalitis virus (TBEV) infection in France was reported in 1968 in Alsace, an eastern region next to the German border: a gamekeeper working in a forest near Strasbourg.1 Between 1970 and 1974, an extensive research survey confirmed the presence of TBEV in ticks and rodents in this French region. Eight percent of adult tick batches collected were infected (Ixodes ricinus) by the TBEV. Tick collection occurred in a forest near Strasbourg, the main city in the region. Nymphs were more rarely infected (1.6% of the collected lots).1 These data were confirmed in 2011 in Alsace in Guebwiller’s Valley, a middle altitude forest, with identification of western (European) subtype TBEV (TBEV-EU). The infection rate still remains low: TBEV was detected only in the I. ricinus nymphs (2.48%) that were collected during May; however, not in those collected during the other spring or summer months. In a more recent study, Bestehorn et al., collected ticks (953 male, 856 female adult ticks and 2,255 nymphs) in endemic foci in the upper Rhine region in France and Germany between 2016, 2017 and 2018 by flagging2. The minimal infection rate (MIR) of the collected ticks in the Foret de la Robertsau (France) was estimated to 0,11% (1 nymph/944 ticks). The isolated and sequenced TBEV strain from Foret de la Robertsau (F) is related to circulating TBEV isolates from eastern Bavaria and the Czech Republic. In the French department Alsace, there are today at least two independent TBEV strains circulating: the historical Alsace strain isolated in 1971 and the newly identified strain from Foret de la Robertsau. Other wooded regions (Ardennes) were explored for TBEV in ticks, but without evidence of virus infection.3
Between 1968 and 2018, more than 200 human tick-borne encephalitis (TBE) cases have been described in France.4,5 The majority of cases (more than 90%) were diagnosed in Alsace. Twenty-two cases were imported, including eight imported cases in 2017.6 Among them, 14 cases came from Germany (after staying in the Black Forest, a mountainous area bordering eastern France). The 8 other imported cases were acquired in Austria, Finland, Poland, Romania, Russia, Slovakia, Sweden, and Switzerland.
Among the autochthonous cases, the majority of the patients were infected in Northeastern France, especially in Alsace (more than 70% of the autochthonous cases during the five last years). Although Alsace remains the area with the highest prevalence of TBE in France, a secondary hotspot was identified in the Alpine region, in a Swiss neighboring area (Savoie and Haute Savoie) during the last ten years with 8 patients presented with TBE. In 2006, 1 patient was infected close to Bordeaux (not a known endemic area). In 2017 and 2018, 3 patients were infected in Haute Loire (in the surrounding countryside of Saint Etienne), making this region a new possible emerging area of TBE, and new foci have been identified in the Auvergne-Rhone region.7 In Alsace, some small areas with higher TBEV endemicity have been identified, especially in the southern Vosges valley, a middle-altitude mountain, and some forests around Strasbourg.4 However, these five last years TBE-diagnosed patients were infected in areas located throughout the region.5
There are currently 3 medical laboratories that test for TBEV in France: the national reference center, the virology laboratory of Strasbourg University Hospital in eastern France, and 1 private laboratory. All 3 of these laboratories participate in the collection of data for any patients diagnosed with TBE as confirmed by the presence of specific TBE immunoglobulin M (IgM) and IgG in serum samples. However, in France, patients with encephalitis are tested for TBE only if they have risk factors (especially travelling to high-endemic regions). Considering Alsace as an endemic region, only patients living in this region are regularly tested for TBE. Only patients with clinical signs compatible with TBE meningoencephalitis are kept for further analyses that are presented here.
Until 2016, in humans, the annual number of cases in France each year ranged from 1 to 12. In 2016 we noticed a recrudescence of infection with 29 cases of TBE infection.5 In 2017 and 2018, 18 and 24 cases were reported, respectively, by the 3 laboratories involved in TBE testing. Except for the year 2017, in 2016 and 2018 more than 80% of the cases were autochthonous. From 2013 to 2018, the transmission period for TBEV is from April to October, with a peak in June and July in half of all cases.
From 2013 to 2017, 60% of the patients presented with meningoencephalitis.6 All patients were hospitalized. The female-to-male ratio was 0.4; mean age was 53 years. Also, 63% of the patients remembered a tick bite during the weeks before the beginning of symptoms that led to TBE diagnosis. Consuming raw milk cheese before the onset of symptoms was recorded for 1 patient, but without any proof that this was the source of the TBEV infection.
Between April and May 2020, a TBE outbreak due to alimentary transmission (non-pasteurized goat milk and milk products) was reported by Santé Publique France in the Auvergne-Rhônes Alpes Region (département de l’ain); data in French available on the web site (www.santepubliquefrance.fr/les-actualites/2020/foyer-de-cas-d-encephalite-a-tiques-lies-a-la-consommation-de-fromage-de-chevre-au-lait-cru-dans-l-ain.-point-au-19-juin-2020). A total of 33 TBE cases were confirmed by the National reference center of arboviruses (Marseille) and 11 are still under investigation. Including these 33 cases results in an estimated total of 68 TBE cases in France in 2020, pending final confirmation. Among the remaining 35 patients, all diagnosed by the laboratory of Virology of Strasbourg University Hospital, the median age was 53.2 years (range: 11–78), 19 of them were male. Transmission occurred by tick bite in 17 (48.6%), it was the alimentary route in 6 (17.14%) and it remained unknown in 12 cases. The 6 additional cases identified as alimentary transmission were all linked to the outbreak previously mentioned above. Only one case was imported (due to COVID-19 lockdown). The two main endemic areas in France are still the Alsace and the Alpine regions.
In 60% of cases, an initial disease stage with fever and flu-like symptoms occurs prior to the onset of meningitis or encephalitis symptoms. Among those cases, 37% had meningitis without any other neurological symptoms and 54.3% had neurological signs associated with meningitis. For 2 patients, a clinical diagnosis of meningo-radiculitis was established.
Between May 2021 and December 2022, 62 cases were notified (31 cases in each year): M/F ratio= 1.6; median age 50 years [IIQ 27–60]; 2 cases were children. 57 cases presented neurological signs: 30 encephalitis or meningoencephalitis, 23 meningitis, 3 encephalomyelitis, and 1 myelitis.
34 cases out of 62 (55%) reported a tick bite before the onset of signs. 52 cases (84%) had acquired their infection in France. Among them, 8 cases (15%) had a job exposing them to tick bites or dairy products made from raw milk from animals at risk. For 6 cases (12%), food contamination in the Auvergne-Rhône-Alpes (ARA) region was suspected:
- Two cases had consumed cheese from the same farm.
- One case worked on a goat farm and reported another case among the employees.
- One case lived on a farm that could not be investigated.
- One case occurred in a breeder whose herd and products were also contaminated.
Two clusters were highlighted in the ARA region in an area not previously known to be at risk.
Overview of TBE in France
| Table 1: Virus, vector, transmission of TBE in France | |
|---|---|
| Viral subtypes, distribution | Western subtype |
| Reservoir animals | Red backed voles (Clethryonomis glareolus) and field mice (Apodemus sylvaticus and A. flavicollis)1 |
| Infected tick species (%)1 |
|
| Dairy product transmission | Possible but unproven5 |
| Table 2: TBE-reporting and vaccine prevention in France | ||
|---|---|---|
| Mandatory TBE reporting | Mandatory reporting planned — expected to be effective in 2022 | |
| Other TBE-surveillance | Mainly three laboratories establish the diagnosis for TBE in France:
The 2020 data above and in the table/graph are those reported by us, the laboratory of Virology of Strasbourg University Hospital, and they are not exhaustive. TBE notification mandatory since May 2021. Case definition: Positive findings with at least one of the following methods:
Probable case definition: the same clinical definition as confirmed cases but with isolated IgM antibody in blood. |
|
| Special clinical features | Approximately 50 % of bi-phasic disease | |
| 1 % mortality | ||
| Available vaccines | Ticovac and Encepur | |
| Vaccination recommendations and reimbursement | Recommendations only for travelers into endemic areas No reimbursement | |
| Vaccine uptake by age group/ risk group/ general population | No information available | |
| Name, address/website of TBE National Reference Center | Arbovirose Reference Center, Institut de Recherche Biomedicale des Armées (Irba), Hôpital d’Instruction des Armées Laveran – Service de Biologie, BP 60149 13384 MARSEILLE CEDEX 13 Laboratoire de Virologie, Hôpitaux Universitaires de Strasbourg, 3, rue Koeberlé, 67000 Strasbourg |
|
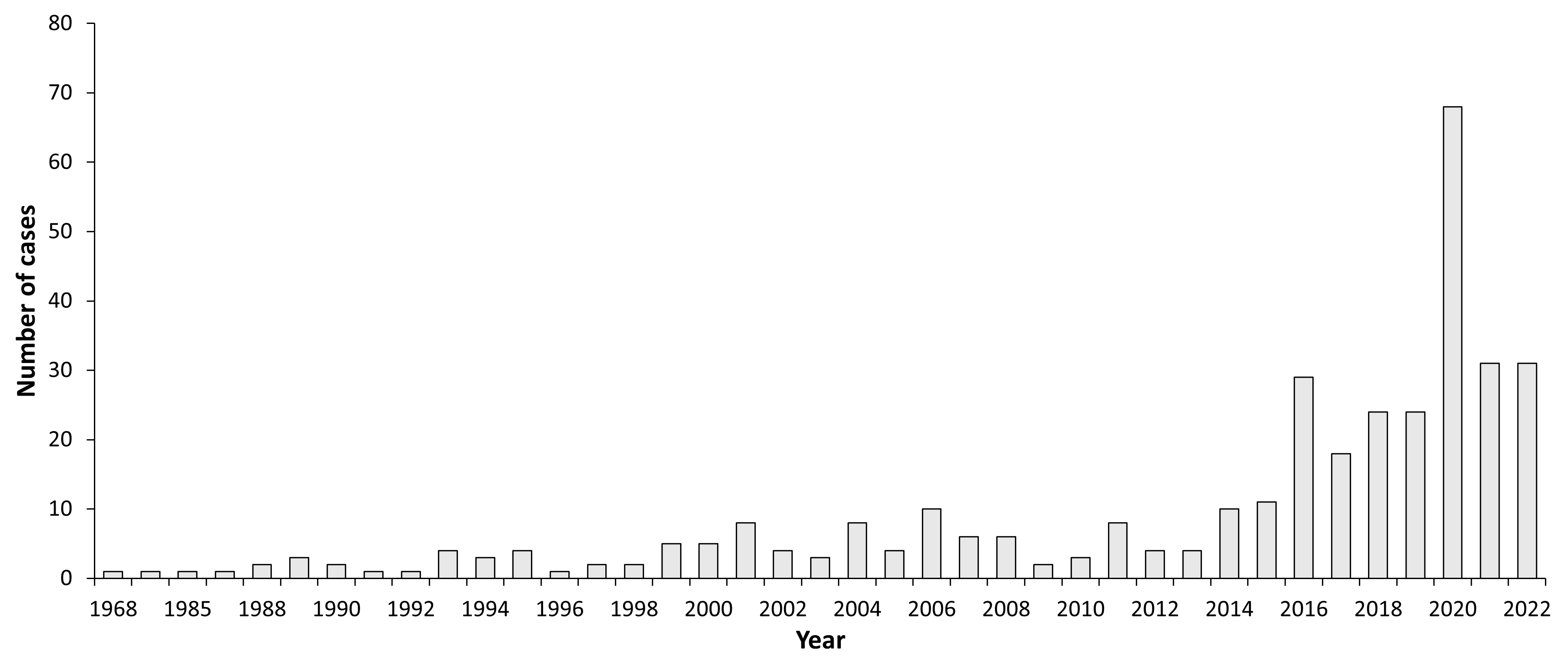
| Year | Number of Cases | Incidence / 105 |
|---|---|---|
| 1968 | 1 | |
| 1970 | 1 | |
| 1985 | 1 | |
| 1986 | 1 | |
| 1988 | 2 | |
| 1989 | 3 | |
| 1990 | 2 | |
| 1991 | 1 | |
| 1992 | 1 | |
| 1993 | 4 | |
| 1994 | 3 | |
| 1995 | 4 | |
| 1996 | 1 | |
| 1997 | 2 | |
| 1998 | 2 | |
| 1999 | 5 | |
| 2000 | 5 | |
| 2001 | 8 | |
| 2002 | 4 | |
| 2003 | 3 | |
| 2005 | 4 | Vaccine available |
| 2006 | 10 | |
| 2007 | 6 | |
| 2008 | 6 | |
| 2009 | 2 | |
| 2010 | 3 | |
| 2011 | 8 | |
| 2012 | 4 | |
| 2013 | 4 | |
| 2014 | 10 | |
| 2015 | 11 | |
| 2016 | 29 | |
| 2017 | 18 | |
| 2018 | 24 | |
| 2019 | 24 | |
| 2020 | 68 | |
| 2021 | 31 | |
| 2022 | 31 |
Figure 2: Age and gender distribution of TBE in France in (2013–2016)5
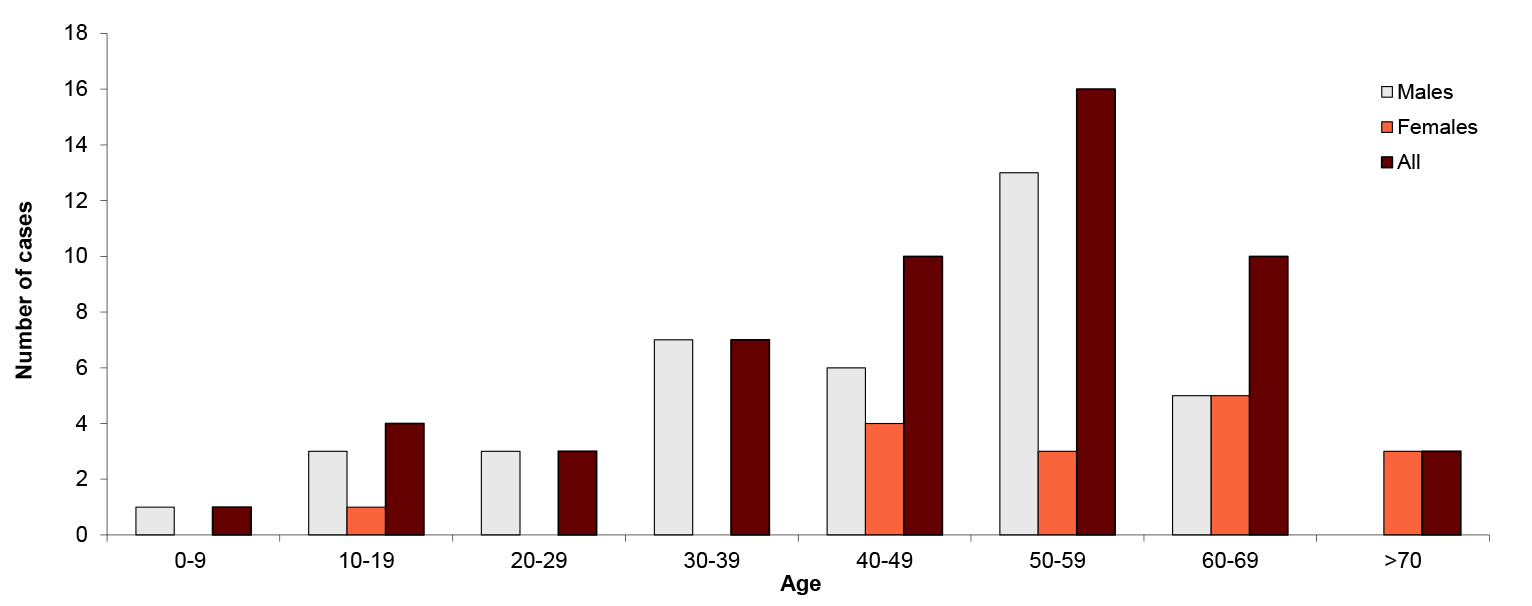
| Age group (years) | Males | Females | All |
|---|---|---|---|
| 0-9 | 1 | 0 | 1 |
| 10-19 | 3 | 1 | 4 |
| 20-29 | 3 | 0 | 3 |
| 30-39 | 7 | 0 | 7 |
| 40-49 | 6 | 4 | 10 |
| 50-59 | 13 | 3 | 16 |
| 60-69 | 5 | 5 | 10 |
| >70 | 0 | 3 | 3 |
Contact:
yves.hansmann@chru-strasbourg.fr
Citation:
Hansmann Y, Velay A. TBE in France. Chapter 12b. In: Dobler G, Erber W, Bröker M, Schmitt HJ, eds. The TBE Book. 6th ed. Singapore: Global Health Press;2023. doi:10.33442/26613980_12b12-6
References
- Perez Eid C, Hannoun C, Rodhain F. The Alsatian tick-borne encephalitis focus: presence of the virus among ticks and small mammals. Eur J Epidemiol. 1992;8:178-86.
- Bestehorn M, Weigold S, Kern WV, et al. Phylogenetics of tick-borne encephalitis virus in endemic foci in the upper Rhine region in France and Germany. PLoS One. 2018;13(10):e0204790.
- Moutailler S, Valiente Moro C, Vaumourin E, et al. Coinfection of ticks: the rule rather the exception. PLoS Negl Trop Dis. 2016;10:e0004539
- Hansmann Y, Pierre Gut J, Remy V, et al. Tick-borne encephalitis in Eastern France. Scand J Infect Dis. 2006;38:520-6.
- Velay A, Solis M, Kack-Kack W, et al. A new hot spot for tick-borne encephalitis (TBE): A marked increase of TBE cases in France in 2016. Ticks Tick Borne Dis, 2018; 9(1):120-125.
- Velay A, Paz M, Cesbron M, et al. Epidémiologie et prévention de l’encéphalite à tique en 2017. 19èmes JNI ; 13-15 juin 2018, Nantes
- Botelho-Nevers E, Gagneux-Brunon A, Velay A, et al. Tick-Borne Encephalitis in Auvergne-Rhône-Alpes Region, France, 2017–2018. Emerg Infect Dis. 2019;25(10):1944–8.
