Andrey Dmitrovskiy
E-CDC risk status: Endemic
(data as of end 2022)
History and current situation
The first isolation of the TBEV in Kazakhstan was achieved in the Almaty region by M.P. Chumakov in 1941 (only one strain from one patient) during the expedition organized by the Central Institute of Epidemiology and Microbiology (Moscow). This is proof that the clinically well-described “spring-summer encephalitis” in the Almaty region was in fact TBE. Later, in 1943, 1944 and 1945 the TBEV was also isolated from additional patients by local scientists from the Institute of Epidemiology and Microbiology, Laboratory of Virology in Alma-Ata by Prof. E. I. Demikhovsky. Isolation had been accomplished from CSF samples up to 8 days of illness and also from brain tissue on day 12.1
In Kazakhstan, the clinical manifestations of TBE were first described by Steblov E.M, again in the Alamty region, and the disease had been named “Almaty encephalitis”. More over, Steblow described a chronic variant of TBE as “Kojevnikov’s Epilepsy”.2 In 1954 the TBEV was isolated from Ixodes persulcatus ticks.3 The endemic zone in Eastern Kazakhstan was first characterized by Zhumatov in 1957.4
In 1959, a total of 5 TBEV strains were isolated from 315 Dermacentor pictus ticks (45% in 11 pools) in Zailiysky Alatau and 12 additional strains in Jungarsky Alatau (720 ticks – 12 pools – 100%).5 In the 1960s the Arbovirus Infections Laboratory of the Institute of Epidemiology, Microbiology and Hygiene (Alma-Ata) under the direction of Prof. Zhumatov conducted extensive work to study the natural foci of TBE in Kazakhstan.
In particular, for several years, they examined birds for TBEV antibodies in Eastern Kazakhstan using a Hemagglutination Inhibition Assay. In 1961, during the examination of the sera of 46 birds, anti-TBEV antibodies were found in 4 local (non-migratory) species of birds (including jackdaw and starling). In 1962, 2 starlings out of 260 were also found with antibodies to the TBEV, whereas testing of 174 farm animal sera turned out to be negative. At the same time, studies of humans in Eastern Kazakhstan demonstrated seropositivity rates from 1.9% to 19.4%.6
The study of human sera in different endemic regions showed that in mountain foci where I. persulcatus is common, antibodies were detected in 12.0% of patients whereas in steppe foci it was 4.7%. Of persons between the ages of 11–15 years, antibodies were detected in 0.7%, between 16–25 years in 7.8%, between 26–35 years in 9.9% and over 35 years in 8.3%.8 When studying human TBEV infection by different genera of ticks in different endemic territories of Kazakhstan, researchers concluded that in those places with no I. persulcatus ticks patients were infected by D. pictus or D. marginatus and such infections did not result in any symptoms of TBE.7
All this work resulted in the creation of an epidemiological surveillance network for TBE, including the annual collection and study of ticks for infection rate, tick treatment of farm and domestic animals, as well as in areas where humans are in areas with a high population density, and in addition vaccination of the population in endemic areas.
Local medical organizations are officially advised to conduct timely identification, recording and reporting of cases, including all individuals affected by tick bites, and this documentation includes diagnostic measures taken, hospitalization, medical examination and treatment of patients with TBE. Clinical supervision for patients who recovered from TBE must be conducted by a neurologist for a two-year period or longer, depending on the patient’s health status. Routine immunization against tick-borne encephalitis must be carried out by medical organizations and must be provided for individuals whose activities are connected with being in a natural focus of TBE.13
The Kazakh Institute of Epidemiology, Microbiology and Hygiene Research defines TBE-endemic areas in the 27 districts and 6 regions of Kazakhstan (Almaty, Eastern Kazakhstan, Akmola, Kostanai, Karaganda and Northern Kazakhstan).13 With no typical TBE cases in steppe foci in recent years, only 15 districts in 2 regions (Almaty and Eastern Kazakhstan)13 are still on the list of TBE-endemic areas. However, in 2016 new cases appeared in “old” endemic zones in the Akmola region.17,18
In 2020, 32 cases were registered, including 6 cases in Akmola and 4 cases in Northern Kazakhstan regions that are not officially endemic. Only one case was registered in the Almaty region and no cases were registered in such major cities as Almaty and Nur Sultan. We explain this by the development of the COVID-19 pandemic and the implementation of restrictive anti-epidemic measures during the tick activity season (April–May), when people could not move freely and travel to endemic zones.
In 2021, the incidence of tick-borne encephalitis continued to decrease (by more than 20% compared to 2020), including a decrease in the number of cases in children (4 and 3 cases, respectively). At the same time, 2021 was characterized by an increase in the number of cases in the “new” endemic territory – the North Kazakhstan region (9 cases compared to 4 in 2020) and the appearance of cases in “non-endemic” territories – Zhambyl region (1 case).
In 2022, the number of confirmed TBE cases has increased to 32 (25% more compared to 2021). The highest number of cases was noted in the Almaty region (together with Almaty city) (13 cases), followed by the East Kazakhstan region (9 cases). The incidence was still registered in the “new” endemic regions – Akmola region (together with Astana, former Nur Sultan, city) with 6 cases, North Kazakhstan region with 3 cases and Zhambyl region with 1 case. Thus, the data of the former Kazakh Institute of Epidemiology on the wider endemicity of TBE, in addition to the Almaty and East Kazakhstan regions, are confirmed. We can also talk about the spread of endemicity in the Zhambyl region.
Overview of TBE in Kazakhstan
| Table 1: Virus, vector, transmission of TBE in Kazakhstan | |
|---|---|
|
Viral subtypes, distribution |
Siberian subtype, Almaty region12 Siberian subtype, Eastern Kazakhstan region13 |
|
Reservoir animals |
No information available |
|
Infected tick species (%) |
By virology studies (1970):14
The tick infection rate of long-term data: In the mountain foci of Zailiyskiy and Dzhungarskiy Alatau (Almaty region)14
The steppe foci of Central Kazakhstan –
The steppe foci of Northern Kazakhstan –
Forest-steppe –
By Elisa on TBEV Ag (2014–2015):15 I. persulcatus 18.6%–21.8% By PCR in Almaty region (2014-2016)16
I. persulcatus 504 ticks/103 pools pos. 22 (21.3%)
I. persulcatus 79/17 pos.5 (29.4%)
I. persulcatus 610/123 pos. 19(15.4%) |
|
Dairy product transmission |
Not documented – rare – frequent |
| Table 2: TBE reporting and vaccine prevention in Kazakhstan | |
|---|---|
|
Mandatory TBE reporting |
Any healthcare worker who has any reason to suspect that the patient has TBE11 A case of tick-borne encephalitis is reported if one of the following is present:17 1) isolation of TBEV from blood or cerebrospinal fluid; 2) detection of TBEV RNA in PCR; 3) detection of IgM to TBEV by ELISA in serum or cerebrospinal fluid; 4) increasing titer of IgG antibodies to TBEV in ELISA A probable case of TBE is reported with acute severe disease, accompanied by high fever, severe intoxication, and a syndrome of meningitis or meningoencephalitis, characterized by at least four of the following: 1) hyperemia and puffiness of face; 2) lethargy or agitation; 3) headache; 4) nausea and vomiting; 5) meningeal symptoms (stiff neck, Kernig’s signs, Brudzinsky’s signs in children) and one – a tick bite; – contact with a tick; – epidemiological link with a confirmed case Possible cases – the definition of a suspected (possible) case in the TBE classification is not being used |
|
Other TBE-surveillance |
Unclear |
|
Special clinical features |
Biphasic disease? Usually no-risk groups? Local population in endemic zones |
|
Available vaccines |
Vaccine tick-borne encephalitis cultural concentrated purified inactivated sorbate “EnceVir” (ЭнцеВир ®) Russia; Suspension for intramuscular injection. 1 dose (0.5 ml) in a vial One dose (0.5 ml) contains inactivated antigen of tick-borne encephalitis virus (TBE) in ELISA titer of at least 1:128 (active component); The course of vaccination consists of two injections with an interval of 1–7 months. Course of vaccination (two vaccinations) can be carried out throughout the year, including during the summer season but not later than two weeks prior to a visit to a TBE endemic zone. The optimal interval between the first and second vaccinations – 5–7 months (autumn-spring). If necessary, emergency prevention, including, at the beginning of vaccinations in the summer, the interval between vaccinations may be reduced to 14 days. |
|
Vaccination recommendations and reimbursement |
Give year when recommendations / reimbursement started, year of changes etc. |
|
Vaccine uptake by age group/ risk group/ general population |
Medical organizations hold preventive, routine immunization against tick-borne encephalitis professionally threatened contingents (risk group) |
|
Name, address/website of TBE National Reference Center |
Scientific practical center for sanitary and epidemiological expertise and monitoring (SPC SEEM), Parasitology Department #84, Auezov street, Almaty, 050008 |
Figure 1: Burden of TBE in Kazakhstan over time
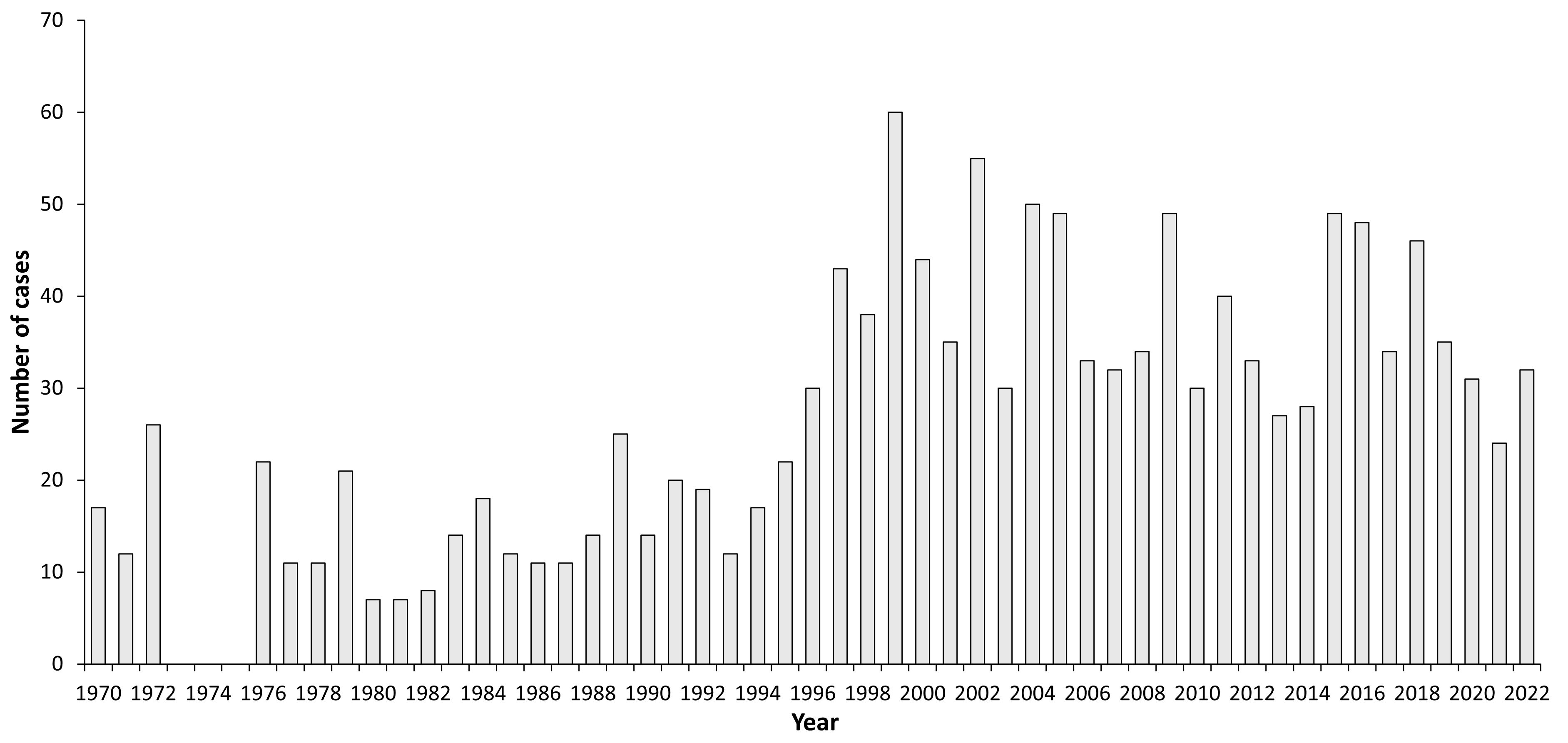
| Year | Number of Cases | Incidence / 105 |
|---|---|---|
| 1970 | 17 | 0.1 |
| 1971 | 12 | 0.09 |
| 1972 | 26 | 0.15 |
| 1973 | ||
| 1974 | ||
| 1975 | ||
| 1976 | 22 | 0.13 |
| 1977 | 11 | 0.07 |
| 1978 | 11 | 0.07 |
| 1979 | 21 | 0.14 |
| 1980 | 7 | 0.04 |
| 1981 | 7 | 0.04 |
| 1982 | 8 | 0.05 |
| 1983 | 14 | 0.09 |
| 1984 | 18 | 0.11 |
| 1985 | 12 | 0.08 |
| 1986 | 11 | 0.07 |
| 1987 | 11 | 0.07 |
| 1988 | 14 | 0.08 |
| 1989 | 25 | 0.2 |
| 1990 | 14 | 0.08 |
| 1991 | 20 | 0.12 |
| 1992 | 19 | 0.13 |
| 1993 | 12 | 0.08 |
| 1994 | 17 | 0.12 |
| 1995 | 22 | 0.15 |
| 1996 | 30 | 0.20 |
| 1997 | 43 | 0.29 |
| 1998 | 60 | 0.41 |
| 1999 | 60 | 0.41 |
| 2000 | 44 | 0.30 |
| 2001 | 35 | 0.23 |
| 2002 | 55 | 0.38 |
| 2003 | 30 | 0.20 |
| 2004 | 50 | 0.33 |
| 2005 | 49 | 0.32 |
| 2006 | 33 | 0.20 |
| 2007 | 32 | 0.21 |
| 2008 | 34 | 0.22 |
| 2009 | 49 | 0.31 |
| 2010 | 30 | 0.20 |
| 2011 | 40 | 0.26 |
| 2012 | 33 | 0.20 |
| 2013 | 27 | 0.18 |
| 2014 | 28 | 0.18 |
| 2015 | 49 | 0.32 |
| 2016 | 48 | 0.31 |
| 2017 | 34 | 0.22 |
| 2018 | 46 | 0.30 |
| 2019 | 35 | 0.19 |
| 2020 | 31 | 0.17 |
| 2021 | 24 | 0.13 |
| 2022 | 32 | 0.17 |
Figure 2: Age and gender distribution of TBE in Kazakhstan
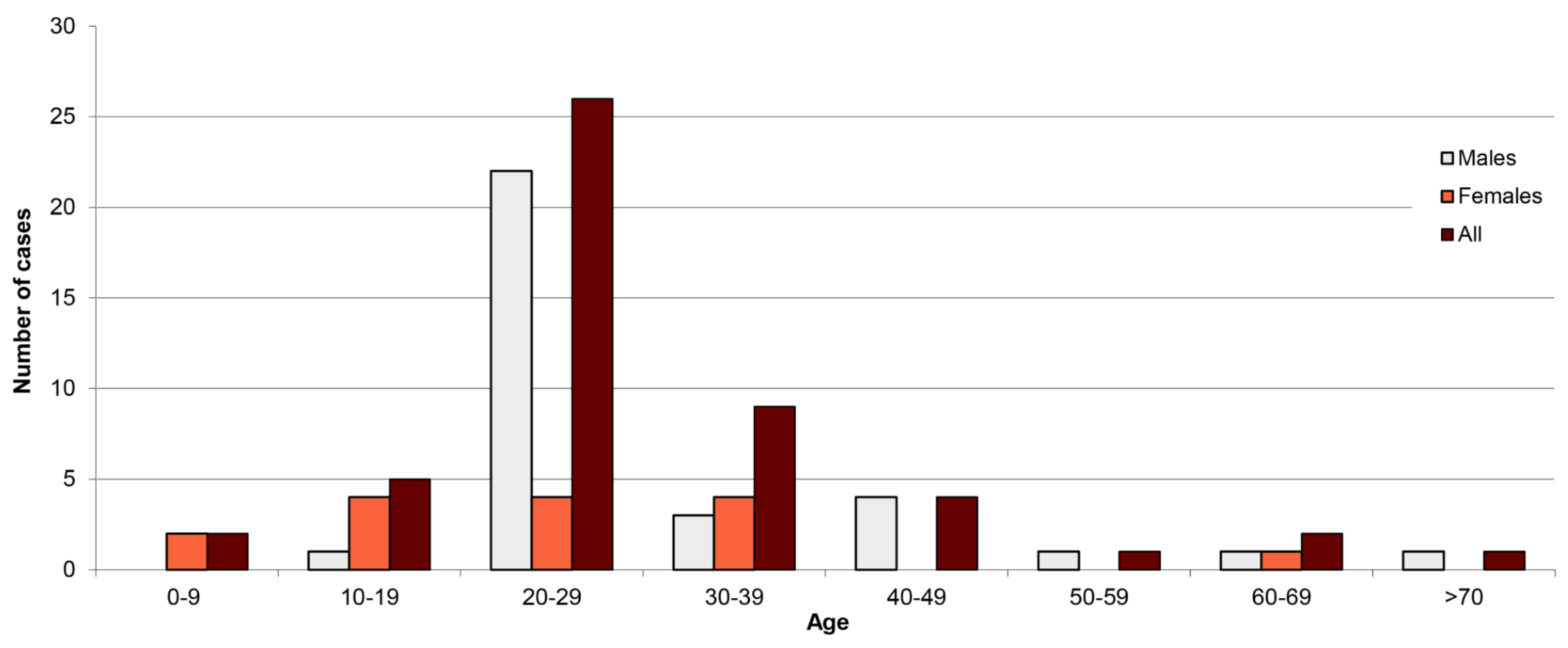
| Age group (years) | Males | Females | All |
|---|---|---|---|
| 0-9 | 0 | 2 | 2 |
| 10-19 | 1 | 4 | 5 |
| 20-29 | 22 | 4 | 26 |
| 30-39 | 3 | 4 | 9 |
| 40-49 | 4 | 0 | 4 |
| 50-59 | 1 | 0 | 1 |
| 60-69 | 1 | 1 | 2 |
| >70 | 1 | 0 | 1 |
Figure 3: TBEV-isolation and TBE cases in Kazakhstan
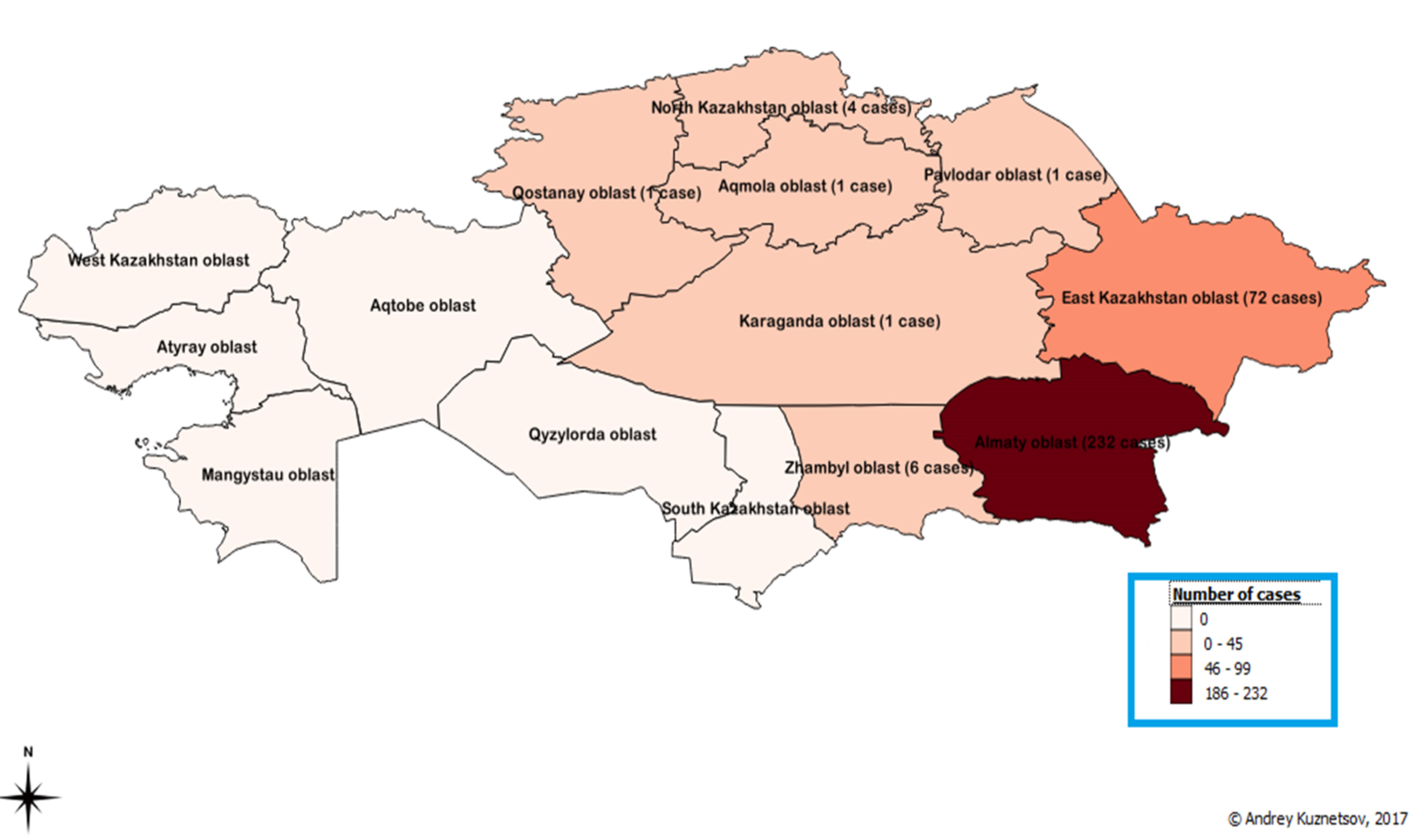
The number of TBE cases in the Regions of Kazakhstan during 1970–1992 (Unfortunately, there is no current information for when and where isolated TBEV was verified, with the exception of the above historical information on the TBEV isolation in Almaty and Eastern Kazakhstan Regions.)
A feature of the epidemiology of tick-borne encephalitis in 2018–2019 was the registration of cases of CE in “unusual” areas-Akmola (9), North Kazakhstan (2), Kostanay (1), Zhambyl (1), and even the appearance of the case in the region where the incidence of TBE has never been recorded before (Kyzylorda-1)
Contact:
am_dimitr@mail.ru
Citation:
Dmitrovskiy A. TBE in Kazakhstan. Chapter 12b. In: Dobler G, Erber W, Bröker M, Schmitt HJ, eds. The TBE Book. 6th ed. Singapore: Global Health Press;2023. doi:10.33442/26613980_12b17-6
References
- Demikhovsky EI. About Almaty virus encephalitis (scientific session). Alma-Ata, 1945:23-24.
- Steblov EM. Clinic, etiology, pathogenesis, differential diagnosis and therapy of Kozhevnikov’s epilepsy (scientific session). Alma-Ata, 1945:24-26.
- Kiryuschenko TV, Akberdin SU. XI Conference of the Kazakh Institute of Epidemiology, Microbiology and Hygiene. Alma-Ata, 1970:123-125.
- Karimov SK, Akberdin SU, Temirbekov TK. Information from the 8th concluding practical science conference of the Kazakh Institute of Epidemiology, Microbiology and Hygiene. Alma-Ata, 1967:65-67.
- Dmitrienko IN, Bondareva RP, Prikhodko ET. Information from the 6th concluding practical science conference of the Kazakh Institute of Epidemiology, Microbiology and Hygiene. Alma-Ata, 1964:39-43.
- Temirbekov ZhT, Akberdin, Tagiltsev AA, Survillo AV, Ustimenko. Information from the 5th concluding practical science conference of the Kazakh Institute of Epidemiology, Microbiology and Hygiene. Alma-Ata, 1963:45,48-51.
- Tagiltsev AA, Dmitrienko IN, Prikhodko ET. Information from the 7th concluding practical science conference of the Kazakh Institute of Epidemiology, Microbiology and Hygiene. Alma-Ata, 1966:90-94.
- Karimov GK, Akberdin, Temirbekov ZhT, Usebayeva TK, Zhumatov. Information from the 8th concluding practical science conference of the Kazakh Institute of Epidemiology, Microbiology and Hygiene. Alma-Ata, 1967:65-68.
- Yegemberdiyeva R. Clinical and epidemiological manifestations of some natural focal vector borne infections in Kazakhstan. Scientific dissertation for the degree of Doctor of Medical Sciences. Chapter 3.3. Characteristic species composition of ticks and their natural infection in the Republic of Kazakhstan. Almaty, 2011:37-47.
- Abdiyeva K. Medical Biodefence Conference. Munich, 2016
- Shapieva ZhZh. (republican SES data) Symposium within the framework of the German-Kazakh partnership in diagnostics of dangerous infectious diseases. Almaty, 2016.
- Abdiyeva KS, Yeraliyeva LT, Turebekov NA, et al. Actual problems of epidemiology, microbiology, natural foci of human diseases. Omsk, 2016:76-78.
- Prikaz [office or department] of the Committee of Health of the Ministry of Education, Culture and Health of the Republic of Kazakhstan dated March 6, 1998; #111 “On preventive measures for the tick-borne encephalitis”.
- Prikaz [office or department] of the Acting Minister of Health of the Republic of Kazakhstan dated December 15, 2006; #623 “About approval of standards of medical practice in identifying cases of especially dangerous infections of humans when they are registering”.
- Prikaz [office or department] of the Acting Minister of Health of the Republic of Kazakhstan dated June 11, 2007; #357 “On approval of sanitary and epidemiological rules and norms. Organization of the sanitary and epidemiological (prophylactic) measures for the prevention of tick-borne encephalitis”.
- Government Decree #89 from January 17, 2012 “On approval of the Sanitary Rules. Sanitary and epidemiological requirements for the organization and conduct of anti-epidemic (preventive) measures for the prevention of parasitic diseases“.
- Yegemberdiyeva R, Shapiyeva Z, Dmitrovskiy A, Oradova A, Azhdarova G, Zhusupov K. Investigation of tick-borne encephalitis spread in the non-endemic regions of Kazakhstan. In: Book of the 16th Medical Biodefense Conference. Munich, 2018:19,51.
- Dmitrovskiy AM. TBE Monitoring and Prophylaxis in Kazakhstan. In: Abstract book of 4th Global Conference on Vaccines Research & Development from February 10-11, 2020 at Lisbon, Portugal. p. 31. doi:10.13140/RG.2.2.33000.62723
- Perfilyeva YV, Shapiyeva ZZ, Ostapchuk YO, et al. Tick-borne pathogens and their vectors in Kazakhstan – A review. Ticks Tick Borne Dis. 2020;11(5):101498. doi:10.1016/j.ttbdis.2020.101498
- Abdiyeva K, Turebekov N, Yegemberdiyeva R, et al. Vectors, molecular epidemiology and phylogeny of TBEV in Kazakhstan and central Asia. Parasit Vectors. 2020;13(1):504. doi:10.1186/s13071-020-04362-1
- Dmitrovskiy A. Case of Nervous System Damage in a Combination of 4 Infections. In: The book of International Webinar on Neurology & Neuro Disorders; December 03-04, 2021:32