Vladimir Igorevich Zlobin, Maria Esyunina and Maria Syrochkina
E-CDC risk status: endemic
(data as of end 2022)
History and current situation
TBE was first revealed in the Far-East Taiga Forest in the Soviet Union in springs and summers between 1933–19351 and it was further investigated as of 1937 at a large multidisciplinary expedition led by Professor Lev Zilber, the Head of the Moscow Medical Virology laboratory.2,3 The expedition demonstrated that the disease develops in humans after a tick bite,4 and the “Taiga Tick” Ixodes persulcatus was established as the virus carrier. The viral etiology of the disease was confirmed and the first strain of TBE virus (TBEV) was isolated. The clinical disease spectrum in humans and the respective pathology were described and the effectiveness of immunoglobulin-therapy was shown.5 Based on morphological studies since 1937 TBE was assigned to the group of neuro-infections as an independent nosological entity.6,7
Vaccines against TBE have been available in Russia since 1939. Already in 1938 Kagan et al. developed the first “mouse brain” formalin-inactivated vaccine from the Far East TBEV subtype “Sof’in” (1st generation of vaccines).17,18 Vaccine impact was established at the level of 98%, but it frequently induced serious adverse events. A live attenuated vaccine based on the Elantsev strain had not been licensed due to severe complications (encephalitis) in the vaccinated group.19 In 1950–1960 a 2nd generation of TBE vaccine was introduced which used chicken embryonic cell culture for virus reproduction.20 The vaccine was upscaled in 1961–1966 and tested in Western Siberia with good real effectiveness. In the1980s another new type of TBE vaccine was licensed and is currently in use, a concentrated purified lyophilized 3rd generation vaccine.21,22
The Siberian subtype dominance of the TBEV (over 60% of endemic areas) in the Russian Federation was demonstrated by numerous virological studies8,9.
Only two species of ticks are epidemiologically significant in Russia: I. persulcatus in the Asian part and some additional areas in the European part (Yaroslavl, Sverdlovsk, Omsk, Irkutsk, Primorsky regions) and I. ricinus in the European part. There is a less epidemiologically significant species – D. pictus – confirmed as a carrier of the TBEV in Udmurtia.10-15
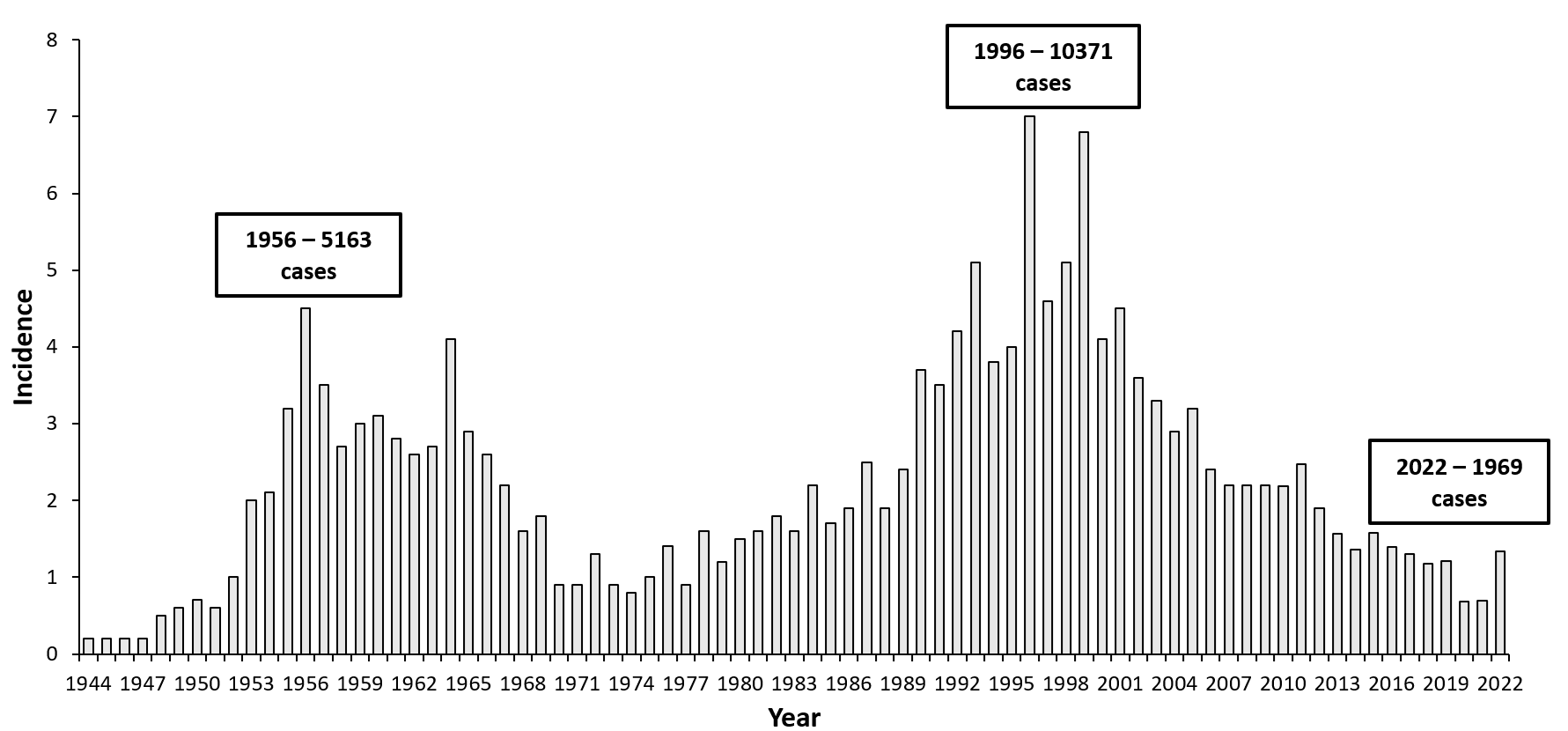
Official reporting of TBE cases in the USSR started in 1944. Fluctuations in TBE incidence had been observed because of the changes within the natural and anthropogenic focies, increased exposure to infected ticks, changes in the social behavior (outdoors activities, extension of the “cultured” areas, etc.), advances in diagnostics and well-designed implemented preventive measures.14 Over time, two disease peaks were observed in Russia (Fig. 1). In the mid-1950s over 5000 cases were reported followed by a gradual decrease of the incidence until 1970. This was explained by human expansion into natural TBE foci as well as by considerable progress in establishing the diagnosis by improved laboratory methods. In 1965–1971 morbidity decreased year by year mainly due to broadly used acaricides (including DDT). From 1972 to 1991, however, morbidity increased again to the level recorded in 1964, because the vector population control had been canceled. Since 1992, a number of socioeconomic factors, including large-scale allotment of land for garden plots and the growing popularity of outdoor activities, have entailed a high risk of tick bites for the urban population. As a result, the indices of TBE morbidity reached the highest values ever recorded.15 TBE peaked in 1996 and 1999 with incidence rates in these years around 7.0 per 100,000 persons, resulting in more than 10,000 cases per year in the country.
In two periods (1997–2006 and 2007–2016) all Russian Federation (RF) endemic regions were divided into three groups with an either low (≤2.9 per 100,000 population), moderate (3.0–8.4 per 100,000) or high (≥8.5 per 100,000) TBE incidence (Figure 2A and B).
Between 1997 and 2006 the average TBE incidence in Russia was 4.0 ± 0.05 per 100,000 totally 58,585 cases in 55 regions of Russia. At that time the number of regions known to be endemic for the disease grew progressively from 41 in 1997 to 47 in 2001 and 2003. The group of regions with a high incidence per 100,000 population included 15 regions, where a total of 48,166 (82.2%) of TBE cases were registered: Tomsk (40.2), Krasnoyarsk (32.6), Udmurt Republic (28.8), Altai (27.0), Khakassia (26.4), Tuva (23.0), Irkutsk (20.9), Kurgan (16.8), Tyumen (15.9), Buryatia (15.3), Perm (13.8), Kemerovo (11.6), Sverdlovsk region (11.0), Novosibirsk (10.8) and Chelyabinsk (8.6). Nine regions were included into the moderate incidence group with 6,482 registered cases (11.1%), i.e. six regions in the European part of Russia [Republic of Karelia (7.6), Kirov (6.6), Vologda (4.5), Kostroma (4.0), Arkhangelsk (3.6) and Novgorod regions (3.2)]; and 3 regions in the Asian part (Altai (5.9), Zabaikalsky (5.6) and Primorsky (5.3) regions). In 28 regions low incidence rates were registered (25 regions in the European part and 3 in the Asian part of Russia).
In 2007–2016 the incidence has been 1.9±0.04 per 100,000 with 27,351 TBE cases registered. During this decade, the most intensive epidemic process occurred in the Asian endemic areas. High incidence rates in the European part of the RF were registered in the Kirov region (8.8%). In the Asian part a cluster was formed between the bordering regions of Altai (16.7), Krasnoyarsk (16.2), Tomsk (16.2), Khakassia (10.6) and Tuva (10.6). Moderate incidence rates were established in 6 regions in the European part and 8 regions in the Asian part, low incidence in 23 regions (Figure 1, B.). In summary, the incidence of TBE in the RF has significantly decreased over the past decade in all regions except in Kirov, where an incidence increase from 6.6 ± 0.7 per 100,000 in 1997–2006 to 8.8 ± 0.8 per 100,000 in 2007–2016 was observed. The registered frequency of tick bites remained constant over time (1944–2016) and is at the level of 400,000–550,000 per year.16
The number of endemic regions of Russia increased from 37 (1956) to 48 (2019). The distribution of TBE in Russia has territorial unevenness, with the largest number of cases recorded in the Siberian Federal District (45%–48% of the total incidence of TBE in the Russian Federation), while in the Volga Region – 17.4%–21.1%, in the Urals – 14%–17%, in the North-West -12.8%–14.3%, in the Central – 2.4%–3.8%, in the Far East – 1.5%–2.2%.
Middle Ural area is an active natural focus of TBE; TBE cases have been recorded since the 1930s. At present, all 94 administrative territories of the Sverdlovsk Region are endemic for the TBE. Sverdlovsk region is a good example of a typical Russian TBE endemic area. In the 1990s in the Sverdlovsk Region TBE changed from an occupational disease to an infection connected to the course of human household activities. TBE incidences in cities began to exceed the incidence in the rural population. Long-term TBE incidence dynamics in the Sverdlovsk region can be separated into 5 periods:
- 1944–1953: the incidence is recorded mainly among rural residents; registered only clinical forms; laboratory diagnostics was absent, there were 100–300 TBE cases annually;
- 1953–1986: TBE incidence increasing; laboratory diagnostics detection of the subclinical (inapparent) forms; increased number of TBE cases in people in the cities; 200–750 TBE cases annually;
- 1986–1989: the period of acaricidal (DDT) air spraying of the forests, TBE incidence decrease, ≤200 TBE cases per year;
- 1990–2000: new TBE incidence increase due to the restoration of the ticks population post-abortion of the acaricidal air spraying. Change in the immune status (both natural immunity obtained after the contact with the virus and adaptive immunity due to vaccination) of the population, change in patients’ characteristics. Identification of subclinical TBE forms, immunization of occupational risk group and start of the routine adult immunization;
- 2000 to present: TBE incidence decrease associated with routine TBE vaccination of the adult population and universal routine immunization of children.26
Given the high incidence of TBE, vaccination has become a leading preventative measure in the Sverdlovsk region. Four tactics of vaccination were realized in Regional Immunization Program (Fig 3):
- 1990–1996 – Selective specific TBE vaccination – immunization of the occupational risk groups;
- 1997–2001 – Adult population routine TBE vaccination;
- 2001–2008 – Routine children ≥7 years of age vaccination and mass immunization of adults;
- 2008 to present – Universal routine vaccination of children from 15 months of age and mass immunization of adults.26
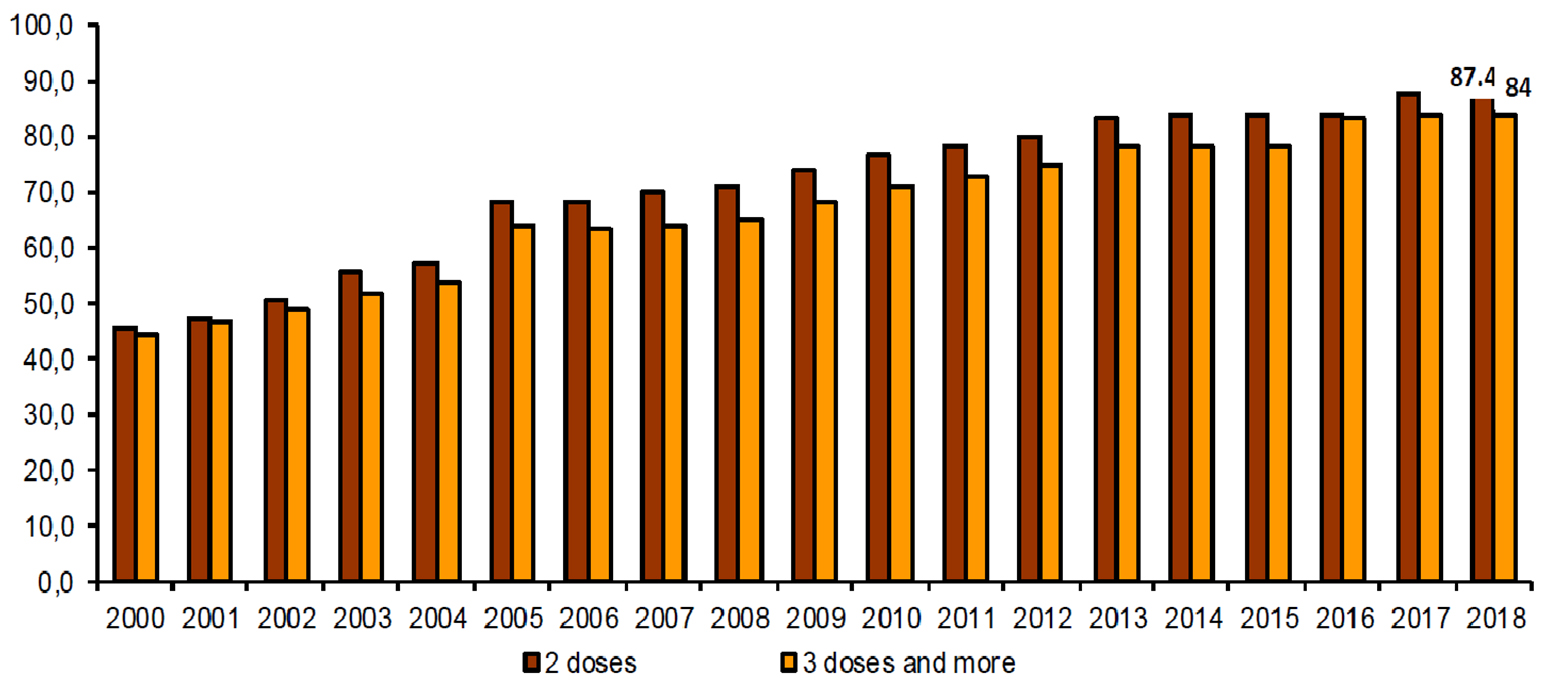
The tactics of universal routine immunization of the population over the age of 15 months in combination with “catch-up” immunization of adults provided an increase in the level of vaccination against TBE from 35 to 87% (Fig. 4) and led to the TBE incidence decrease. 98% TBE vaccination field effectiveness in 2016 (Fig. 6).26,27,28
To summarize current TBE data from Russia, in 2020 there were 471,630 visits30 (in 2019 – 580,069 visits; in 2018 – 518,510 visits; in 2017 – 509,323 visits) to medical centers due to a tick-bite with ~25% of the cases occurring in children; were registered 967 cases of TBE (0.66 per 100,000), in 2019 – 1,781 cases of TBE (1.2 per 100,000), in 2018 – 1,727 cases of TBE (1.18 per 100,000), in 2017 – 1934 cases (1.3 per 100,000). There is a current tendency of TBE incidence reduction in the Russian Federation. In the period 2007–2019, 265 people died from TBE, in 2020 – 18 deaths.24-25,29-30
In 2019 in Russia primary and booster series of TBE vaccines were administered to 3.2 million people. In the last 6 years, the planned annual immunization rates have not exceeded 3.3 million people per year, which is about 4 times lower than required due to insufficient awareness and absence of a national immunization program – regions are purchasing vaccine themselves according to the local budget available (Fig. 6).23,24,25
The means of nonspecific prevention is common to all tick-borne infections. Acaricidal treatment of endemic territories by special substances (cipermetrin 25% or analogues) is regarded to be the main measure nowadays. Compared with 2011, these measures were more than doubled, when in 2016 in the RF over 17,600,000 m2 of the most populated regions and areas actively used by people areas (i.e., parks, camps and recreation zones, hospitals, hotels, schools and kindergarten territories) were deployed in endemic regions.23
Overview of TBE in Russia
| Table 1: Virus, vector, transmission of TBE in Russia | |
|---|---|
| Viral subtypes, distribution | European , Siberian, and Far Eastern TBEV subtypes |
| Reservoir animals | Vertebrate reservoir animals assumed |
| Infected tick species (%) | 6.3% infected ticks from people after tick bite 5.7% infected ticks from natural foci |
| Dairy product transmission | Rare (goat, cow milk) |
| Table 2: TBE reporting and vaccine prevention in Russia | |
|---|---|
| Mandatory TBE reporting | TBE case definition: Any person who has had a tick bite and who has been in the endemic area of TBE during a tick activity period or who has consumed goat milk and has symptoms of CNS inflammation (e.g., meningitis, meningo-encephalitis, encephalomyelitis) or fever. Laboratory criteria for case confirmation:TBE specific IgM or/and IgG antibodies in blood Seroconversion or four-fold increase of TBE-specific antibodies in paired serum samples. Virology is performed in ticks only – ELISA or multiplex PCR for TBEV, Borrelia burgdorferi sl, Anaplasma phagocytophilum, Ehrlichia chaffeensis / Ehrlichia muris |
| Other TBE-surveillance | Endemicity definition: The territory is considered endemic for TBE with the combined presence of the following components:
or:
or:
(Source: Sanitary regulations “Prevention of tick-borne encephalitis” 3.1.3.2352-08) |
| Special clinical features | 1%–10% – TBEV meningoencephalitis or meningoencephalomyelitis, 35%–40% – TBEV meningitis 35%–40% – fever+ anti-TBEV IgM or IgG increase 1%–3% – chronic TBEV with no reliable data available on neurological sequelae Mortality rate 1%–2% Risk groups: permanent inhabitants and visitors of endemic areas; mainly acquired during leisure activities, occupational risk groups (Source: Sanitary regulations “Prevention of tick-borne encephalitis” 3.1.3.2352-08) |
| Available vaccines | Russian TBE vaccines: – Klesch-E-Vac for children 0.25 ml and for adults 0.5 ml (FEDERAL STATE BUDGETARY SCIENTIFIC INSTITUTION Chumakov Federal Scientific Center for Research and Development of Immune-and- Biological Products of Russian Academy of Sciences, Moscow) (Source: http://chumakovs.ru/en/products) – Tick-borne encephalitis vaccine concentrated purified inactivated adsorbed culture dry 0.5ml (FEDERAL STATE BUDGETARY SCIENTIFIC INSTITUTION Chumakov Federal Scientific Center for Research and Development of Immune-and- Biological Products of Russian Academy of Sciences, Moscow) – EnceVir®Neo for children 0.25 ml (NPO Microgen, Tomsk) – EnceVir ® for adults 0.5 ml (NPO Microgen, Tomsk) (Russian vaccines have booster every 3 years) European vaccines: – Encepur adult 0.5ml (Bavarian Nordic, Germany) – Encepur baby 0.25ml (Bavarian Nordic, Germany) – FSME-IMMUN 0.5ml (Pfizer, Austria) – FSME-IMMUN junior 0.25ml (Pfizer, Austria) (Source: http://www.microgen.ru/en/) |
| Vaccination recommendations and reimbursement | National immunization Calendar for epidemic indications (Order of the Ministry of Health of the Russian Federation №125n, part 2): endemic regions have the right to implement local immunization program (RIP) with vaccination rates determined by financial conditions in the region (universal vaccination or vaccination of risk groups only – i.e., infants and elderly) Vaccination is indicated for – persons living in endemic areas (all ages) – persons with occupational risk (forest workers, etc.) – persons travelling to endemic areas(Sanitary regulations “Prevention of tick-borne encephalitis” 3.1.3.2352-08; Ministry of Health Order #125-n part 2 “National Immunization Calendar for epidemic indications”) |
| Name, address/website of TBE National Reference Center | Irkutsk Anti-Plague Research Institute of Rospotrebnadzor, Irkutsk, Russian Federation (Source: http://irknipchi.ru) |
Figure 1: TBE incidence in Russia (all regions, endemic and non-endemic) in 1944–2022 per 100,000 population
| Year | Number of Cases | Incidence / 105 |
|---|---|---|
| 1944 | n/a | 0.2 |
| 1945 | n/a | 0.2 |
| 1946 | n/a | 0.2 |
| 1947 | n/a | 0.2 |
| 1948 | n/a | 0.5 |
| 1949 | n/a | 0.6 |
| 1950 | n/a | 0.7 |
| 1951 | n/a | 0.6 |
| 1952 | n/a | 1 |
| 1953 | n/a | 2 |
| 1954 | n/a | 2.1 |
| 1955 | n/a | 3.2 |
| 1956 | n/a | 4.5 |
| 1957 | n/a | 3.5 |
| 1958 | n/a | 2.7 |
| 1959 | 3516 | 3 |
| 1960 | n/a | 3.1 |
| 1961 | n/a | 2.8 |
| 1962 | n/a | 2.6 |
| 1963 | n/a | 2.7 |
| 1964 | n/a | 4.1 |
| 1965 | n/a | 2.9 |
| 1966 | n/a | 2.6 |
| 1967 | n/a | 2.2 |
| 1968 | n/a | 1.6 |
| 1969 | n/a | 1.8 |
| 1970 | 1169 | 0.9 |
| 1971 | 1175 | 0.9 |
| 1972 | 1707 | 1.3 |
| 1973 | 1189 | 0.9 |
| 1974 | 1062 | 0.8 |
| 1975 | 1336 | 1 |
| 1976 | 1883 | 1.4 |
| 1977 | 1220 | 0.9 |
| 1978 | 2184 | 1.6 |
| 1979 | 1649 | 1.2 |
| 1980 | 2072 | 1.5 |
| 1981 | 2221 | 1.6 |
| 1982 | 2513 | 1.8 |
| 1983 | 2248 | 1.6 |
| 1984 | 3115 | 2.2 |
| 1985 | 2423 | 1.7 |
| 1986 | 2728 | 1.9 |
| 1987 | 3620 | 2.5 |
| 1988 | 2774 | 1.9 |
| 1989 | 3528 | 2.4 |
| 1990 | 5475 | 3.7 |
| 1991 | 5194 | 3.5 |
| 1992 | 6239 | 4.2 |
| 1993 | 7571 | 5.1 |
| 1994 | 5640 | 3.8 |
| 1995 | 5935 | 4 |
| 1996 | 10371 | 7 |
| 1997 | 6804 | 4.6 |
| 1998 | 7531 | 5.1 |
| 1999 | 10011 | 6.8 |
| 2000 | 6010 | 4.1 |
| 2001 | 6569 | 4.5 |
| 2002 | 5231 | 3.6 |
| 2003 | 4773 | 3.3 |
| 2004 | 4178 | 2.9 |
| 2005 | 4593 | 3.2 |
| 2006 | 3433 | 2.4 |
| 2007 | 3142 | 2.2 |
| 2008 | 3140 | 2.2 |
| 2009 | 3141 | 2.2 |
| 2010 | 3094 | 2.18 |
| 2011 | 3533 | 2.47 |
| 2012 | 2716 | 1.9 |
| 2013 | 2236 | 1.57 |
| 2014 | 1978 | 1.36 |
| 2015 | 2304 | 1.58 |
| 2016 | 2035 | 1.39 |
| 2017* | 1934 | 1.3 |
| 2018** | 1727 | 1.18 |
| 2019*** | 1775 | 1.21 |
| 2020 | 989 | 0.67 |
| 2021 | 1015 | 0.69 |
| 2022 | 1969 | 1.34 |
*State Report “About the sanitary-hygiene wellbeing of the population of the Russian Federation in 2017” http://rospotrebnadzor.ru/documents/details.php?ELEMENT_ID=10145
**State Report “About the sanitary-hygiene wellbeing of the population of the Russian Federation in 2018” https://www.rospotrebnadzor.ru/documents/details.php?ELEMENT_ID=12053
***State Report “About the sanitary-hygiene wellbeing of the population of the Russian Federation in 2019” https://www.rospotrebnadzor.ru/documents/details.php?ELEMENT_ID=14933
Figure 2: TBE incidence (per 100,000 population) in the Russian Federation 1997–2006 (А) and 2007–2016 (B)
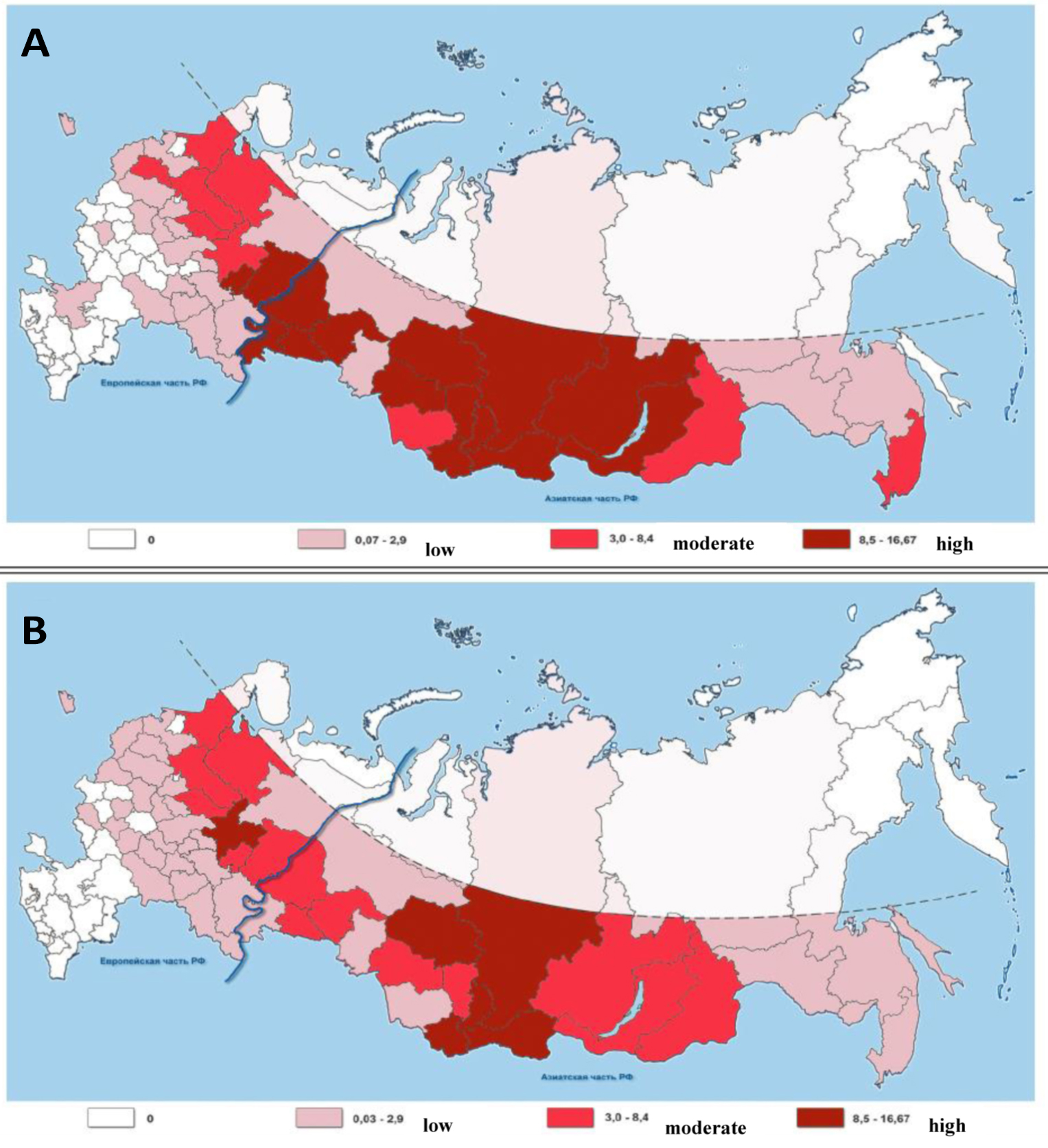
Figure 3: TBE Incidence in Sverdlovsk region by preventive tactics period in 1990–2018 (per 100,000 population, children under 14 years old)
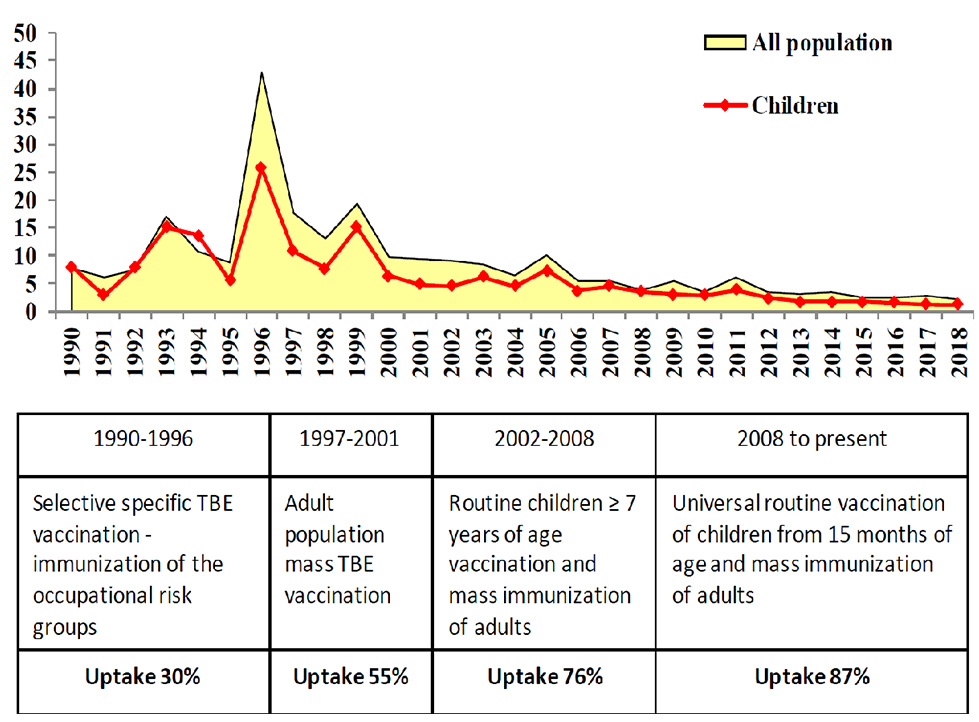
Figure 5: TBE incidence in vaccinated and unvaccinated persons in 2000-2016 in Sverdlovsk region (per 100,000 vaccinated/unvaccinated populations)
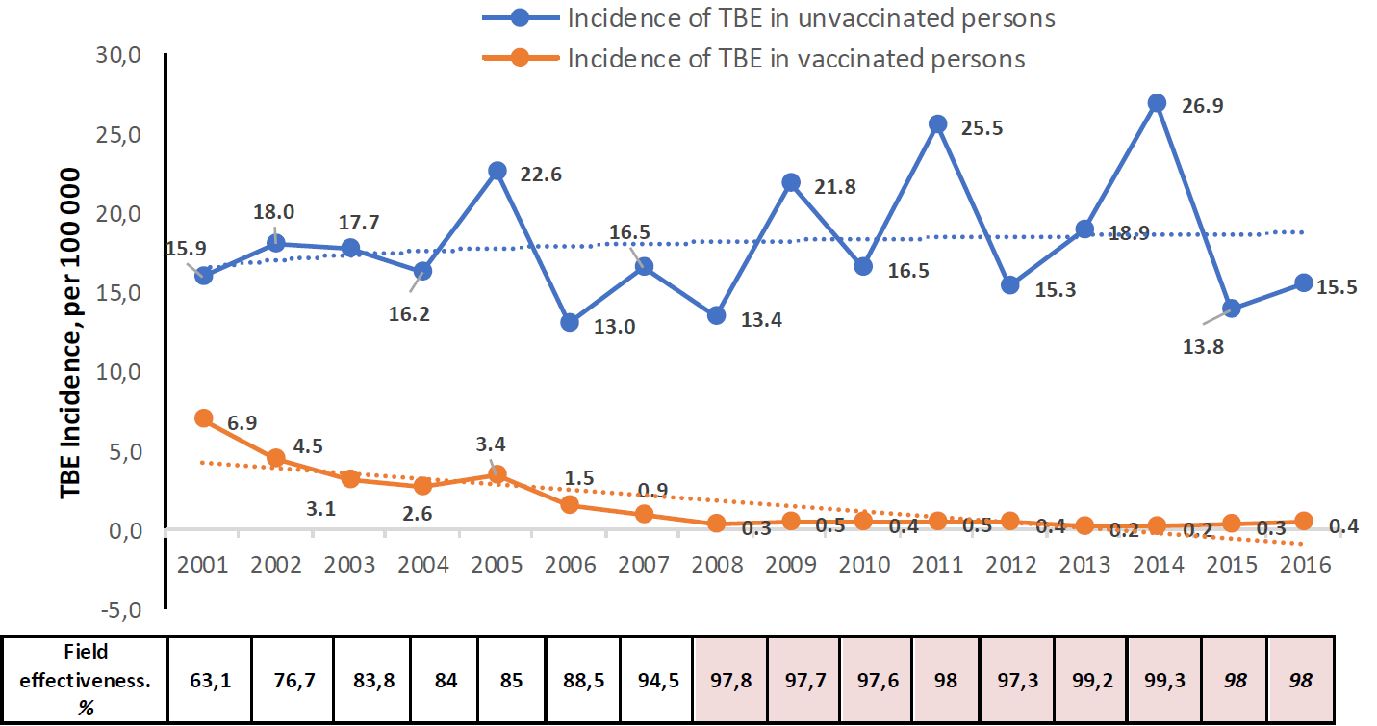
Figure 6: Incidence of tick bite cases per 100,000 population, population seroprotection by vaccination (%), and rate of tick infection (ELISA, %) in the Russian Federation between 2009–2016
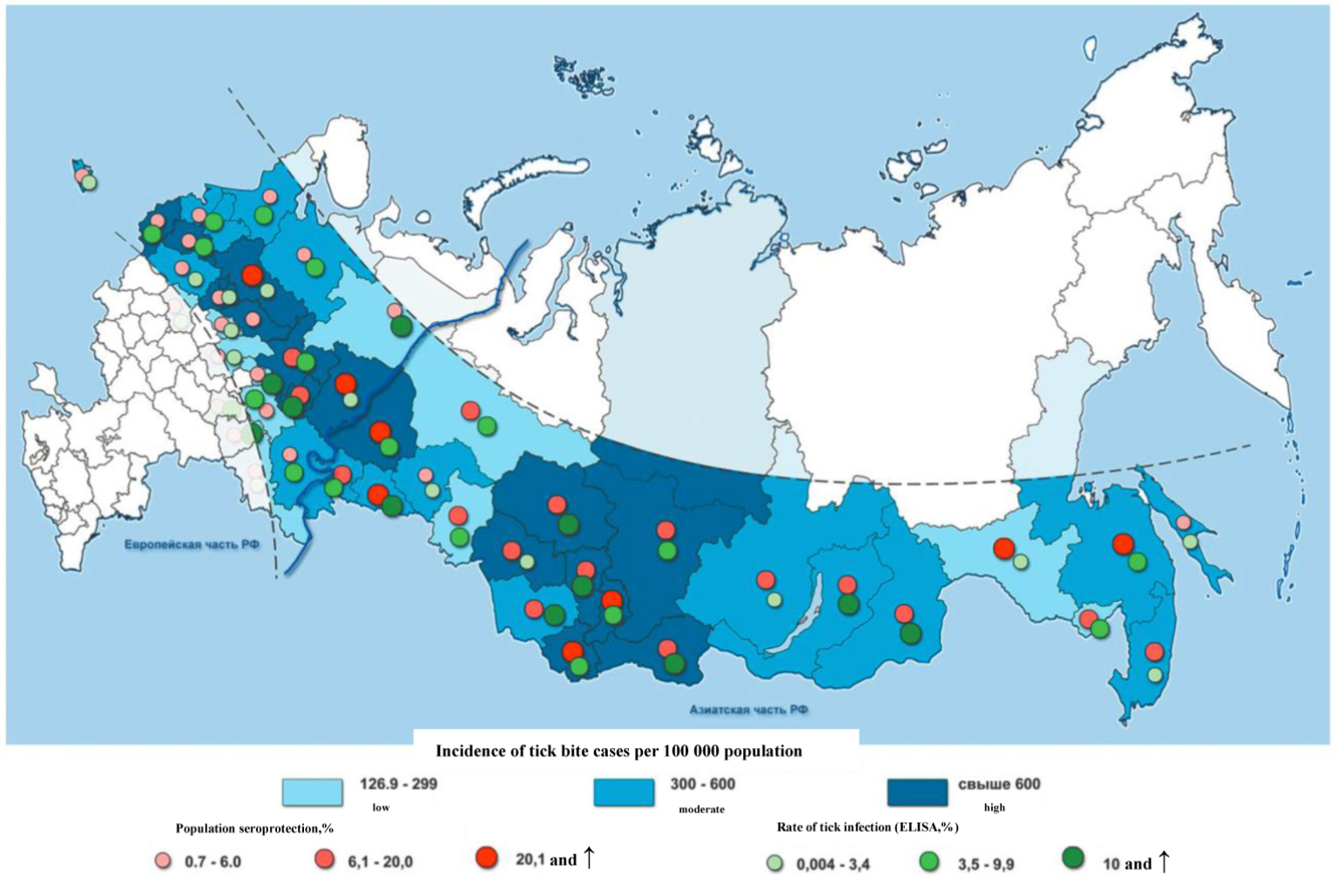
Table 3: Age distribution of TBE in Russia (2016–2019)*
| 2016 | ||
|---|---|---|
| Age | Number of Cases | Incidence / 10 5 |
| Up to 1 year | 3 | 0.16 |
| 1-2 years | 19 | 0.50 |
| 3-6 years | 85 | 1.21 |
| 7-17 years | 165 | 1.04 |
| ≥18 years | 1763 | 1.50 |
| All | 2035 | 1.39 |
| 2017 | ||
| Age | Number of Cases | Incidence / 10 5 |
| Up to 1 year | 2 | 0.10 |
| 1-2 years | 10 | 0.26 |
| 3-6 years | 76 | 1.05 |
| 7-17 years | 148 | 0.90 |
| ≥18 years | 1698 | 1.45 |
| All | 1934 | 1.30 |
| 2018 | ||
| Age | Number of Cases | Incidence / 10 5 |
| Up to 1 year | 2 | 0.10 |
| 1-2 years | 14 | 0.36 |
| 3-6 years | 48 | 0.64 |
| 7-17 years | 139 | 0.83 |
| ≥18 years | 1524 | 1.3 |
| All | 1727 | 1.18 |
| 2019 | ||
| Age | Number of Cases | Incidence / 10 5 |
| Up to 1 year | 1 | 0.06 |
| 1-2 years | 26 | 0.7 |
| 3-6 years | 79 | 1.03 |
| 7-17 years | 149 | 0.87 |
| ≥18 years | 1520 | 1.3 |
| All | 1775 | 1.21 |
Contact:
vizlobin@mail.ru
Citation:
Zlobin V, Esyunina M, Syrochkina M. TBE in Russia. Chapter 12b. In: Dobler G, Erber W, Bröker M, Schmitt HJ, eds. The TBE Book. 6th ed. Singapore: Global Health Press;2023. doi:10.33442/26613980_12b27-6
References
- Chumakov MP. Tick-transferred spring-summer encephalitis in the European part of the USSR and Western Siberia. Zoolog J. 1940;19(2):335
- Zilber LA. To the history of Far-East encephalitis investigations. Vopr Virusol. 1957;(6):323-331
- Pogodina VV. The 70th anniversary of discovery of TBE. A path to true history. Vopr Virusol. 2007;52(5):5-8 [In Russian]
- Zlobin VI. TBE: etiology, epidemiology and prevention problems in the beginning of the XXI century. Ural Medical Journal – special issue “Microbiology”. 2006;6-11 [In Russian]
- Pogodina VV. “Memories of Elizabeth Nikolaevna Levkovich” – M. 2001;201 [In Russian]
- Volkova LI. Pathomorphosis of acute TBE in the Sverdlovsk region. Short PhD thesis – Perm. 2001;34 [In Russian]
- Volkova LI, Romanenko VV, Struin NL, et al. Epidemiology, etiology, clinical presentation, diagnosis, treatment and prevention of TBE. Methodological instructions – Yekaterinburg. 2004;4-51 [In Russian]
- Zlobin VI, et al. Molecular epidemiology of TBE. Vopr Virusol. 2007;52(6):4-9 [In Russian]
- Zlobin VI, Demina TM, Mamaev LV, et al. Analysis of TBEV genetic variability by the primary structure of the surface E-protein gene. Vopr Virusol. 2001;1:13-16 [In Russian]
- Gerasimov SG, Druzhinina TA, Karan LS, Kolyasnikova NM, Baranova NS, Levina LS, Malenko GV, Pogodina VV, Bochkova NG. Features of TBE in the Yaroslavl region at the present stage. The problem of the evolution of infection. Epidemiol Infect Dis. 2014;19(4):37-44 [In Russian]
- Glinsky NP, Kokorev VS, Patsuk NV, Kuchkova EV, Gogoleva OYu. Tick-borne encephalitis: epidemiology, clinic, diagnosis, prevention – Yekaterinburg: AMB Publishing House. 2006; p. 164 [In Russian]
- Danchinova GA, Khasnatinov MA, Zlobin VI. Ixodid mites in the south of Eastern Siberia and Mongolia and their spontaneous infection with pathogens of natural focal transmissible infections. Bulletin of Siberian Medicine – Tomsk. 2006;5(1):137-143 [In Russian]
- Alekseev AN, Dubinina EV, Yushkova OV. Functioning of “tick-causative agents” parasitic system in conditions of increasing anthropogenous pressure. S-Peterburg: Insanta; 2008. 146 p.
- Korenberg E.I., Pomelova V.G., Osin N.S. [Natural focal infections transferred by Ixodes ticks]. М.: “Nauka”; 2013. 463 p.
- Korenberg E, Likhacheva T. Analysis of the long-term dynamics of tick-borne encephalitis (TBE) and ixodid tick-borne borrelioses (ITBB) morbidity in Russia. Zentralbl Bakteriol. 2006;296(S1):54–58
- Noskov AK, Nikitin AYa, Andaev EI, Pakskina ND, Yatsmenko EV, Verigina EV, Balakhonov SV. Tick-Borne Virus Encephalitis in the Russian Federation: Features of Epidemic Process in Steady Morbidity Decrease Period. Epidemiological Condition in 2016 and the Forecast for 2017. Problems of Particularly Dangerous Infections. 2017; 1:37–43. (In Russ.). DOI: 10.21055/0370-1069-2017-1-37-43
- Smorodintsev AA, Dubov AV. TBE and its prevention by vaccination. Leningrad: Medicine. 1986; p. 232 [In Russian]
- Smorodintsev AA, Levkovich EN, Dankovskiy NL. Epidemiological effectiveness of active immunization against TBE. JMEI. 1941;4:12 [In Russian]
- Levkovich EN, Zasukhina GD, Chumakov, et al.. Tissue culture vaccine against TBE. Vopr Virusol. 1960;2:233-236 [In Russian]
- Lvov DK. Immunoprophylaxis of TBE. Doctoral thesis. Moscow, 1965 [In Russian]
- Bilalova GP, Bystritsky LD, Vorobyova MS, Krasilnikov IV. The history of vaccine production for the prevention of tick-borne encephalitis in the city of Tomsk: from brain vaccine to EnceVir vaccine. Bull. Sib. Dep. RAMS. 2007;4:105-110 [In Russian]
- Vorovich MF, Hapchaev Yu Kh, Prilukova NS, Nagirieva LI, Grachev VP. Russian inactivated dry vaccine against tick-borne encephalitis. Biomedicines. 2004;2(14):17-20 [In Russian]
- State Report “About the sanitary-hygiene wellbeing of the population of the Russian Federation in 2016”. Available at: http://www.rospotrebnadzor.ru/bitrix/redirect.php?event1=file&event2=download&event3=gosudarstvennyy-doklad-2016.pdf&goto=/upload/iblock/0b3/gosudarstvennyy-doklad-2016.pdf
- State Report “About the sanitary-hygiene wellbeing of the population of the Russian Federation in 2017”. Available at: http://rospotrebnadzor.ru/documents/details.php?ELEMENT_ID=10145
- State Report “About the sanitary-hygiene wellbeing of the population of the Russian Federation in 2018”. Available at: https://www.rospotrebnadzor.ru/bitrix/redirect.php?event1=file&event2=download&event3=gosudarstvennyy-doklad-zashchita-prav-potrebiteley-v-rossiyskoy-federatsii-v-2018-godu.pdf&goto=/upload/iblock/332/gosudarstvennyy-doklad-zashchita-prav-potrebiteley-v-rossiyskoy-federatsii-v-2018-godu.pdf
- Esyunina MS. Current trends in the incidence of tick-borne encephalitis in various tactics of vaccination and the improvement of epidemiological surveillance and control. PhD dissertation, Perm, 2015; p. 146 [In Russian]
- State report “On the state of sanitary and epidemiological well-being population in the Sverdlovsk region in 2017”. Available at: http://www.66.rospotrebnadzor.ru/c/document_library/get_file?uuid=0091fbe2-bfaa-4cc0-9eaa-1e8a91053b58&groupId=10156 [In Russian]
- State report “On the state of sanitary and epidemiological well-being population in the Sverdlovsk region in 2018”. Available at: http://www.66.rospotrebnadzor.ru/c/document_library/get_file?uuid=cffb1abc-98c1-48aa-8a30-044b2b04c2c1&groupId=10156 [In Russian]
- State report “On the state of sanitary and epidemiological well-being of the population of the Russian Federation the in 2019”. Available at: https://www.rospotrebnadzor.ru/documents/details.php?ELEMENT_ID=14933 [In Russian]
- Report 2 “Information about infectious and parasitic diseases” 2020 Data of the Federal Center for Hygiene and Epidemiology