Zoran Simonović and Tamara Vuković Janković
ECDC risk status: endemic
(data as of end 2022)
History and current situation
TBE is endemic in Slovenia, and the incidence rate is one of the highest in the EU. In Slovenia, TBE virus was confirmed for the first time in 1953 with isolation of the virus from a patient’s blood.1 In 1955, the virus was isolated from a tick Ixodes ricinus.2
Notification of TBE cases as well as deaths due to TBE has been mandatory in Slovenia since 1977. Only cases with central nervous system involvement and laboratory confirmation are notified. Surveillance data has been collected within the communicable diseases surveillance system by the National Institute of Public Health of Slovenia (NIPH).
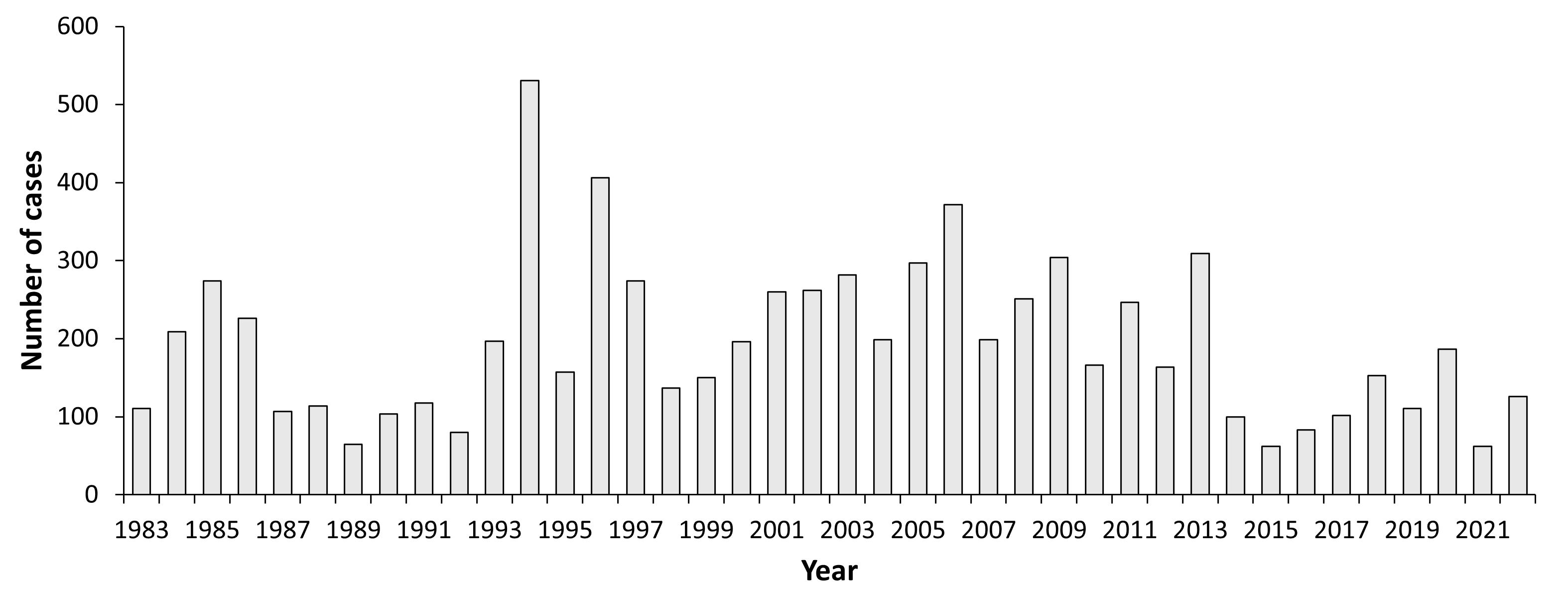
The number of TBE reported cases in Slovenia varies every year. In the period from 1983 to 2016, the number of annually reported TBE cases was between 62 and 531 (incidence rates between 3.0 and 26.6/100,000), which amounts to a mean of 206 cases/year, and a mean annual incidence rate of 10.3/100.000. In contrast to reports on increasingly higher incidence rates of TBE during the last two decades from many endemic countries, in Slovenia the reported incidence rates during the last 35 years have shown no apparent increasing or decreasing trend. Occurrence of the disease presumably fluctuates due to climatic factors influencing tick activity and population number of small forest mammals, different weather conditions during summer months in different years and other possible factors (e.g., changes in leisure activities) that have not been investigated yet.
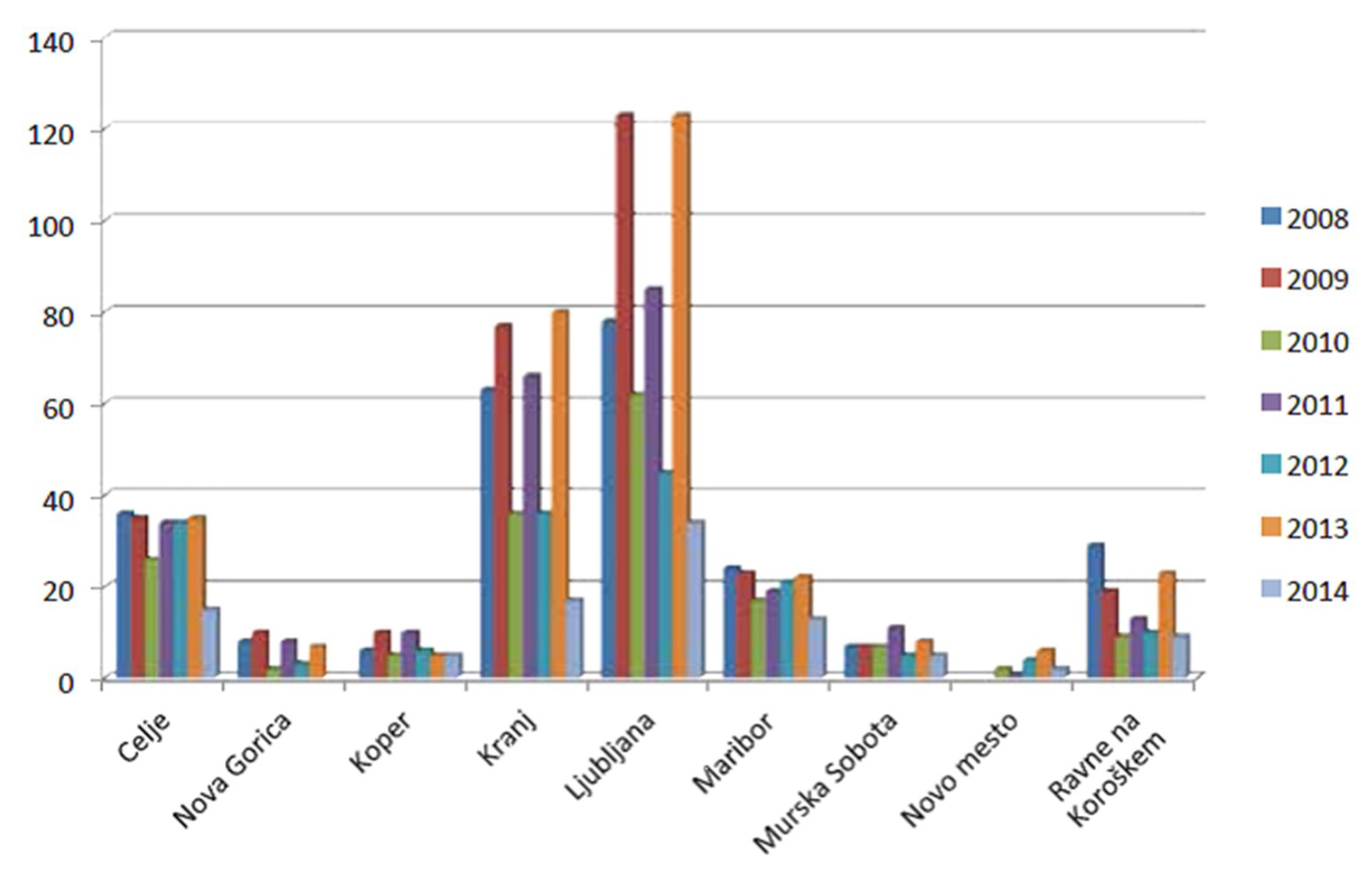
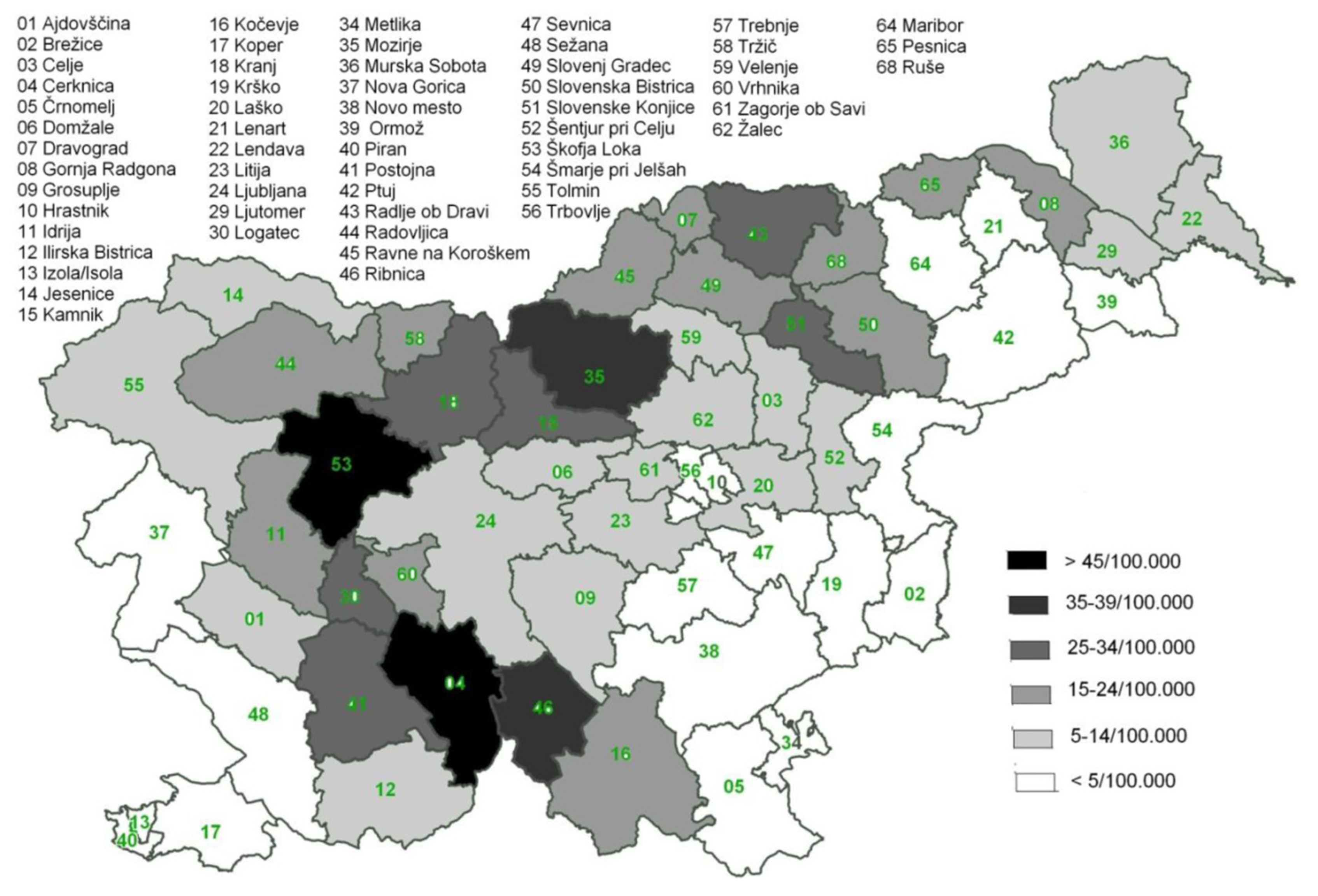
TBE virus is present in all Slovenian regions. Although some regions in Slovenia have higher incidence of TBE than others, TBE occurs throughout the country, with the most affected areas in the north and central regions (Figure 1). In some administrative units average annual TBE incidence rates exceed 45/100,000 (Figure 2).
TBE infections occur seasonally, in Slovenia mostly between April and November, with a peak in June and July.5 In the recent years an increase of the cases in the elderly has been observed. Since 1994, TBE incidence rates have been the highest in the 55–64 age group in most years, with males being more frequently affected than females.6 In men, the 65–74 age group and in women the 45–54 age group followed, with the second highest rates in most years. In contrast to the TBE incidence, the disease burden expressed in DALYs was higher in children aged 5–14 years than in adults aged 50–74 years.7
People who are staying in the endemic areas (temporarily or permanently) have a higher risk for TBE infection. These are mainly people working in forestry, wood and wood-processing industries and construction. The risk is also higher among farmers, if their farmlands are located near forested areas, which present a natural habitat for ticks. There have also been observations of increased TBE incidence among people who visit forests for recreational purpose or forest fruit-picking. An epidemiological study that included 1,564 cases of TBE in Slovenia showed that 82.3% of cases had a tick bite on one or multiple sites on the body. The estimated duration of tick attachment was less than 6 h in 23.5% of TBE cases. Long attachments (more than 24 h) were reported by 10% of the patients. The tick bite occurred while the TBE patients were engaged in leisure time activities (sports or camping, 32.8%), mushroom or berry picking (30.2%), or farming (23.3%). Almost two-thirds of TBE patients reported that they had practiced at least one of the recommended preventive measures, most frequently self-inspection, and least often repellent use.8
Overview of TBE in Slovenia
| Table 1: Virus, vector, transmission of TBE in Slovenia | |
|---|---|
| Viral subtypes, distribution | European subtype; great heterogeneity of the viruses with geographical clustering of viruses with the same genetic characteristics.9 |
| Reservoir animals | Rodents; TBE virus antibodies were detected in 5.9% of rodent sera. Bank voles had higher rate of infection than mice.10 |
| Infected tick species (%) | In Slovenia the main vector is Ixodes ricinus and the prevalence of TBE ticks infection is 0.47%.11 |
| Dairy product transmission | Cases of alimentary TBE 2012–2014: 6 (4 in small outbreak in 2012).12 |
| Table 2: TBE reporting and vaccine prevention in Slovenia | |
|---|---|
| Mandatory TBE reporting13,14 | Reporting is mandatory. Only confirmed cases are reported formally to clinicians.Clinically diagnosed CNS infection of TBE must be confirmed by at least one of the following:
|
| Other TBE-surveillance | – |
| Special clinical features | – |
| Available vaccines | FSME-Immun and Encepur.15 |
| Vaccination recommendations and reimbursement16,17,18,19,20 | TBE vaccination was introduced in 1986. National TBE vaccination policy and recommendation implemented only for high-risk groups:
In 2019, the vaccination against TBE, funded by the Health Insurance Institute of Slovenia, is available to children born in 2016 and adults born in 1970. Vaccination is performed by selected personal physicians or paediatricians. |
| Vaccine uptake by age group/ risk group/ general population | In 2007, general population aged 15 years and more who reported ever to have been vaccinated against TBE was 12.4 %. No further estimations of vaccine coverage have been performed. In 2014, according to official data from National Institute of Public Health of Slovenia, the number increased to 16%. No further estimates of vaccine coverage have been performed.18 |
| Name, address/website of TBE National Reference Center | National Institute of Public Health of Sloveniahttp://www.nijz.si/en |
Figure 3: Burden of TBE in Slovenia over time3,4
| Year | Number of Cases | Incidence / 105 |
|---|---|---|
| 1983 | 111 | 5.56 |
| 1984 | 209 | 10.47 |
| 1985 | 274 | 13.72 |
| 1986 | 226 | 11.32 |
| 1987 | 107 | 5.36 |
| 1988 | 114 | 5.71 |
| 1989 | 65 | 3.26 |
| 1990 | 104 | 5.21 |
| 1991 | 118 | 5.91 |
| 1992 | 80 | 4.01 |
| 1993 | 197 | 9.87 |
| 1994 | 531 | 26.59 |
| 1995 | 157 | 7.86 |
| 1996 | 406 | 20.33 |
| 1997 | 274 | 13.72 |
| 1998 | 137 | 6.86 |
| 1999 | 150 | 7.51 |
| 2000 | 196 | 9.82 |
| 2001 | 260 | 13.02 |
| 2002 | 262 | 13.12 |
| 2003 | 282 | 14.12 |
| 2004 | 199 | 9.97 |
| 2005 | 297 | 14.90 |
| 2006 | 372 | 18.63 |
| 2007 | 199 | 9.90 |
| 2008 | 251 | 12.40 |
| 2009 | 304 | 14.90 |
| 2010 | 166 | 8.10 |
| 2011 | 247 | 12.00 |
| 2012 | 164 | 8.00 |
| 2013 | 309 | 15.00 |
| 2014 | 100 | 4.90 |
| 2015 | 62 | 3.00 |
| 2016 | 83 | 4.00 |
| 2017 | 102 | 4.90 |
| 2018 | 153 | 7.60 |
| 2019 | 111 | 4.21 |
| 2020 | 187 | 9.35 |
| 2021 | 62 | 2.94 |
| 2022 | 126 | 5.97 |
Figure 4: Age and gender specific incidence rates of TBE in Slovenia in year 20183
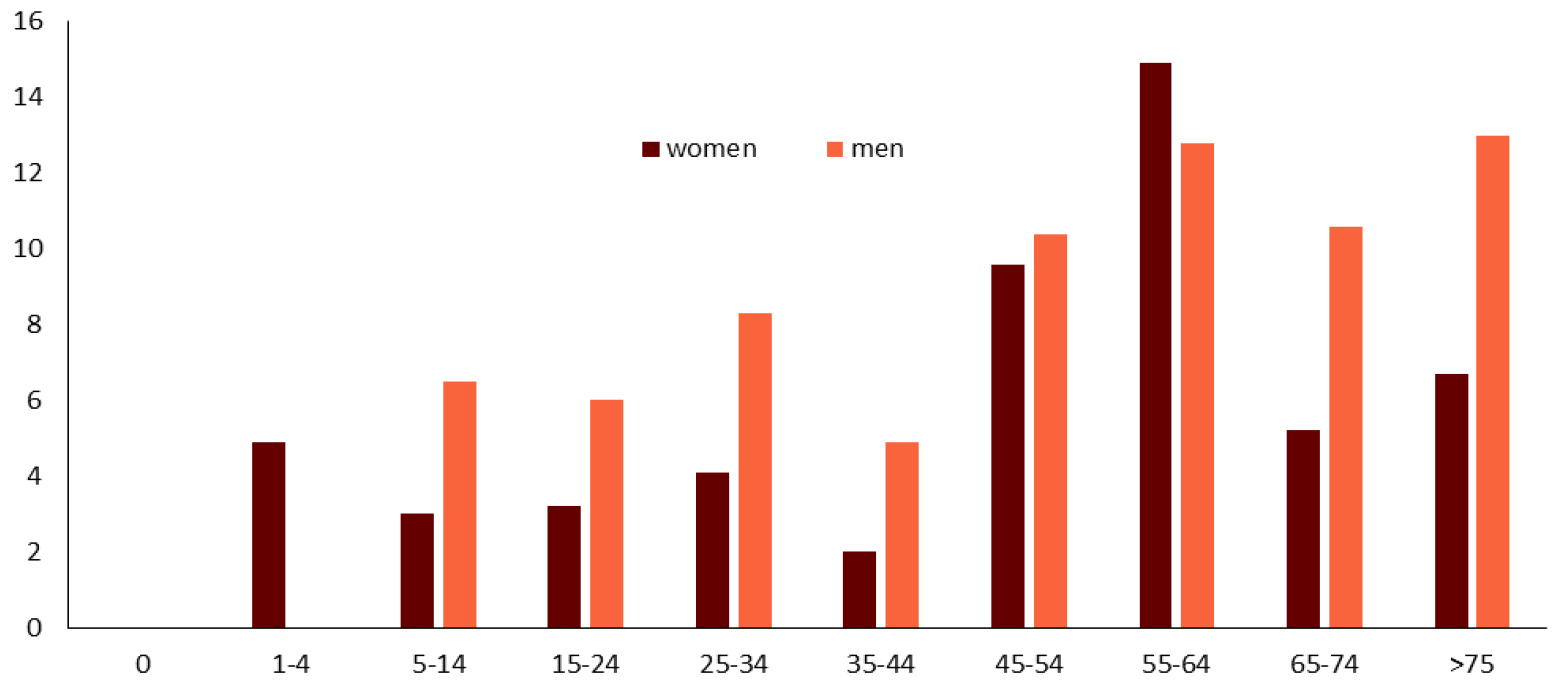
Figure 5: Mean annual incidence per 100,000 of tick-borne encephalitis, by age and gender, Slovenia, 2009–20138
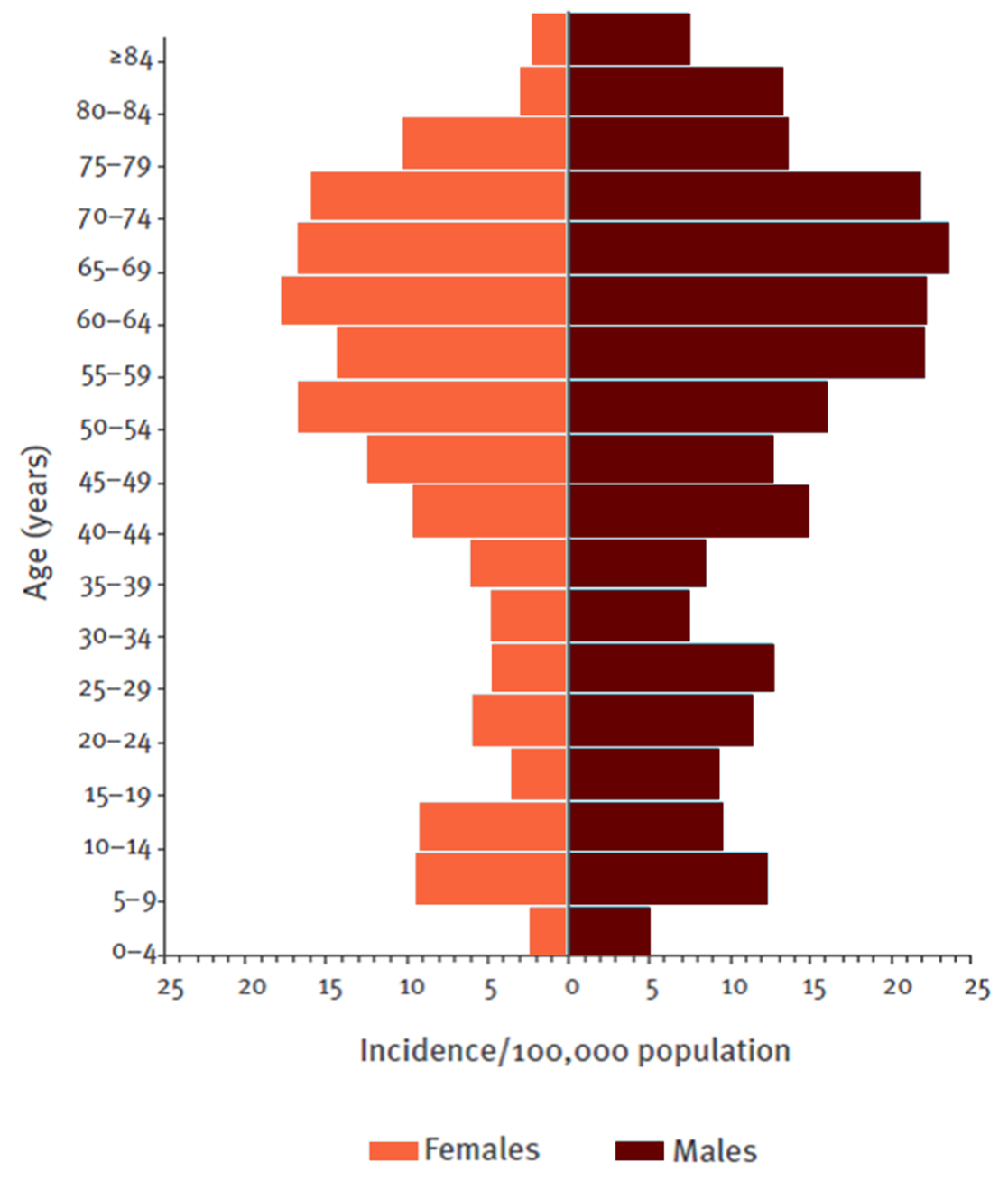
Figure 6: Geographical distribution of TBE virus isolation from rodents only, 2005–2008. TBEV-isolation in Slovenia10
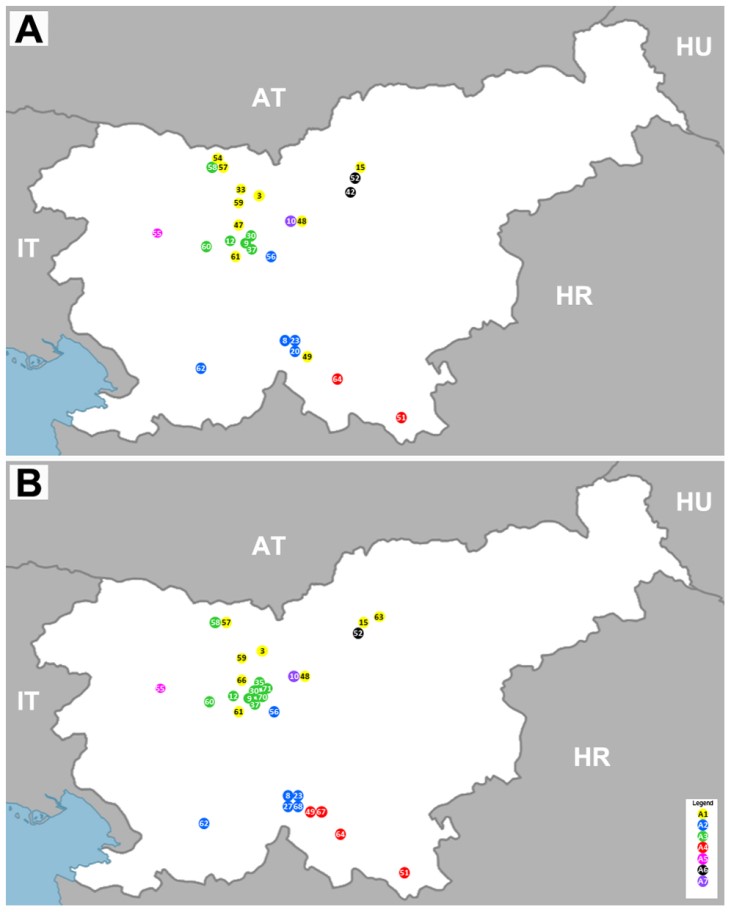
Figure 7: Map of municipalities in Slovenia, showing sites where tick-borne encephalitis virus (TBEV) was detected in rodents (represented in dots) and municipalities (gray coloured) where rodents were captured (2000–2008).

Contact:
Zoran.simonovic@nijz.si
Citation:
Simonović Z, Vuković-Janković T. TBE in Slovenia. Chapter 12b. In: Dobler G, Erber W, Bröker M, Schmitt HJ, eds. The TBE Book. 6th ed. Singapore: Global Health Press;2023. doi:10.33442/26613980_12b30-6
References
- Vesenjak-Zmijanac J, Bedjanič M, Rus S, Kmet J. Virus meningoencephalitis in Slovenia: isolation of the causative agent. Bull WHO. 1955;12:513-20.
- Likar M, Kmet J. Virus meningo-encephalitis in Slovenia: isolation of the virus from the ticks I. ricinus. Bull WHO. 1956;15(1-2):275-9.
- NIJZ podatkovni portal, Available at: http://www.nijz.si/sl/klopni-meningoencefalitis-razsirjenost-in-zascita [Accessed April 2017]
- Vitek-Grgič M. Epidemiologija klopnega meningoencefalitisa in humane granulocitne anaplazmoze v Sloveniji. Klinika za infekcijske bolezni in vročinska stanja, UKC Ljubljana. Klopni meningoencefalitis in humana granulocitna anaplazmoza. 2014;1:17-24.
- Kraigher A, Matjašič M, Hočevar-Grom A, Turk K. TBE surveillance in Slovenia. Antibiotica Monitor. 1996;12:121-3.
- Grgič-Vitek M, Klavs I. High burden of tick-borne encephalitis in Slovenia – challenge for vaccination policy. Vaccine. 2011;29:5178-83.
- Fafangel M, Cassini A, Colzani E, Klavs I, Grgič Vitek M, Učakar V, et al. Estimating the annual burden of tick-borne encephalitis to inform vaccination policy, Slovenia, 2009 to 2013. Euro Surveill. 2017;22:30509.
- Blasko-Markic M, Socan M. Tick-borne encephalitis in Slovenia: data from a questionnaire survey. Vector Borne Zoonotic Dis. 2012;12:496-502.
- Fajs L, Durmiši E, Knap N, Strle F, Avšič-Županc T. Phylogeographic characterization of tick-borne encephalitis virus from patients, rodents and ticks in Slovenia. PloS One. 2012;7:1-8
- Knap N, Korva M, Dolinšek V, Sekirnik M, Trilar T, Avšič-Županc T. Patterns of Tick-Borne Encephalitis Virus Infection in Rodents in Slovenia. Vector Borne Zoonotic Dis. 2012;12:236-42.
- Durmiši E, Knap N, Saksida A, Trilar T, Duh D, Avšič-Županc T. Prevalence and molecular characterization of tick-borne encephalitis virus in i. ricinus ticks collected in Slovenia. Vector Borne Zoonotic Dis. 2011;11:659-64.
- Hudopisk N, Korva M, Janet E, Simetinger M, Grgič-Vitek M, Gubenšek J, et al. Tick-borne encephalitis associated with consumption of raw goat milk, Slovenia, 2012. Emerg Infect Dis. 2013;19:806-8.
- Sočan M, Šubelj M. Definicije prijavljenih nalezljivih bolezni za namene epidemiološkega spremljanja. Ljubljana : Inštitut za varovanje zdravja Republike Slovenije, 2012.
- Simonović Z. TBE epidemiology in Slovenia, Poster 17th ISW TBE Meeting, 29 – 30 January 2015, Vienna.
- Database of medicines in Slovenia. Available at: http://www.cbz.si/cbz/bazazdr2.nsf/Search?SearchView&Query=(%5BSIATCKLA%5D=J07BA01*)&SearchOrder=4&SearchMax=301 [Accessed July 2017]
- Zavadska D, Anca I, André F et al. Recommendations for tick-borne encephalitis vaccination from the Central European Vaccination Awareness Group (CEVAG). Hum Vaccin Immunother. 2013;9:362–74.
- NIPH. Program cepljenja in zaščite z zdravili za leto 2016. Ljubljana : Nacionalni inštitut za javno zdravje, 2016. Available at: : http://www.nijz.si/sl/program-cepljenja-inzascite-z-zdravili-za-leto-2016 [Accessed June 2017]
- Grgič-Vitek M, Klavs I. Low coverage and predictors of vaccination uptake against tick-borne encephalitis in Slovenia. Eur J Public Health. 2012;22:182-6.
- NIPH. Recommendations for vaccination against tick-borne meningoencephalitis, May 30th, 2019. Available at: https://www.nijz.si/sites/www.nijz.si/files/uploaded/kme-priporocila_za_cepljenje_proti_kme_2019_maj.pdf [Accessed March 2020]
- NIPH. Frequently Asked Questions and Answers on Introducing TBE Vaccination into the Vaccination Program. Available at: https://www.nijz.si/sl/najpogostejsa-vprasanja-in-odgovori-o-uvedbi-cepljenja-proti-kme-v-program-cepljenja [Accessed March 2020]