Yang Junfeng and Heinz-Josef Schmitt
ECDC risk status: endemic
(no new data available as of May 2023)
History and current situation
The first TBE patients in China were reported in 1943, and the TBEV was isolated from the brain tissues of 2 patients in 1944 by Japanese military scientists,1 and from patients and ticks (Ixodes persulcatus and Haemaphysalis concinna) in 1952 by Chinese researchers.2 The Far Eastern viral subtype (TBEV-FE) is the endemic subtype that has been isolated from all 3 known natural foci (northeastern China, western China, and southwestern China).14 Recently a new “Himalayan subtype” of the TBEV (TBEV-HIM) was isolated from wild rodent Marmoata himalayana in the Qinghai-Tibet Plateau.15 The main vector of the TBEV in China is I. persulcatus.3 One recent report suggests that the TBEV-SIB is prevalent in the Uygur region (North West China)13 but epidemiological modelling indicates that the TBEV may occur even widely all over China (Figure 3).4 Likely, the disease is often missed by clinicians due to a lack of the availability of specific diagnostic assays.16
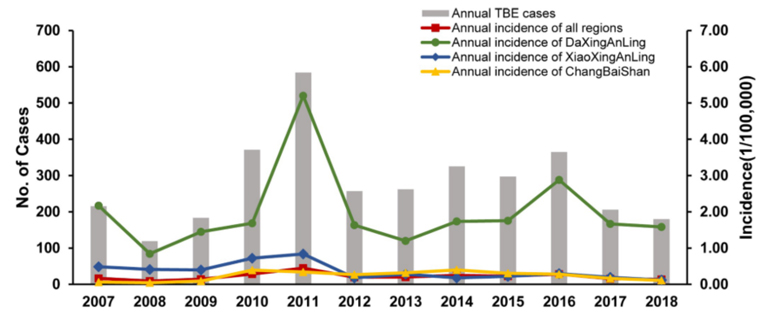
Serological research has demonstrated that there are high numbers of human TBEV-infections in the 3 foci mentioned above. However, TBE patients are mainly reported from northeastern China, including Inner Mongolia Autonomous Region (Daxing’an Mountains), Heilongjiang Province (Xiaoxing’an Mountains), and Jilin Province (Changbai Mountains). In a recent report 803 cases including 4 deaths were reported from the Jilin Province with most cases from the Changbai Mountains and neighboring areas.17 Interestingly, 61.5% of patients were farmers and this is different from previous reports where soldiers and forest workers made up the majority of patients. The most recent publication of the Chinese CDC18 reports 3,364 TBE cases in China between 2007 and 2018 (incidence 0.09 – 0.44/105). Overall only 14%–84% of cases were laboratory confirmed. Given the extremely high percentage of TBE-infected ticks as well as the high seroprevalence in humans (table 1), TBE numbers may be hugely underreported.
Patients also were reported from another important epidemic area: the Tianshan Mountains and Altai Mountains of the Xinjiang Autonomous Region.4
Despite the small geographic distribution, the whole belt that connects the 3 above-mentioned foci is considered to be at risk (E-CDC status: predisposed) for occurrence of TBE if the virus is imported, including a few densely populated regions such as Beijing, Shaanxi, and Sichuan provinces, where the environment could be suitable for circulation of TBEV (see Figure 3). In addition, cases may be missed in regions with lower TBE incidences due to a lack of awareness among both physicians and the general population.15
The incidence of TBE decreased in China during the 1980s, but has been rising in recent years, as noted by disease control and prevention authorities and local hospitals.4 TBE patients were mainly forest workers before the 1980s, however, it has been reported that changes in the occupation/type of “exposure risk” occurred among TBE patients since the 1980s and in particular since the late 1990s, with 70%–95% of the most recent patients being non-forest working farmers, housewives, domestic workers, students, or anyone with any occupation who entered endemic forest areas.5
Overview of TBE in China
| Table 1: Virus, vector, transmission of TBE in China | |
|---|---|
| Viral subtypes, distribution | Far Eastern TBEV subtype (TBEV-FE) |
| Reservoir animals | Mice and insectivorous animals; migratory birds; lagomorphs, goats6 |
| Infected tick species (%) | Ixodes persulcatus; however, TBEV has also been isolated from Haemaphysalis concinna, H. japonica, Dermacentor silvarum, and I. ovatus5 |
| Infection rate among the ticks | 13.0%–14.3%, 0.79%–6.45%, and 0%–37.5% in northeastern China; 14.3%–47.7% in northwestern China; 8.3% in southwestern China4 |
| Dairy product transmission | Not known |
| Serological infection rate in healthy people | 19.7% in southwestern China,6 35.4% in northwestern China,7 0%–10.9%,8 0%–9.8%,9 7.6% in northeastern China10 |
| Table 2: TBE reporting and vaccine prevention in China | |
|---|---|
| Mandatory TBE reporting | Heilongjiang Province only |
| Other TBE-surveillance | No |
| Special clinical features | Biphasic disease not reported in China. Different symptoms among patients with different disease severities. In the early 1950s, case fatality rate (CFR) of TBE in the northeastern forest areas was over 25%, but since the 1980s it has decreased to around 8%.1,2,11 Long-lasting sequelae of TBE are common, almost one-third of the patients in the 1952 outbreak had paralysis in the neck muscles or the shoulder muscles.2 Recently, the complications of TBE over a 10-year period reported to be 16.6% (90/542).12 |
| Available vaccines | TaiSenBao produced in China with Sen-Zhang strain as seed strain in primary hamster kidney (PHK) cells |
| Vaccination recommendations and reimbursement | No |
| Vaccine uptake by age group/ risk group/ general population | No information available, estimated to be low |
| CFR | 25% in 1950s, and decreased to <10% after 1980s1,2,11 |
| Name, address/website of TBE National Reference Center | Chinese Center for Disease Prevention and Control: http://ivdc.chinacdc.cn/ |
Figure 2: Gender-related distribution of TBE cases in China, 2007–201818
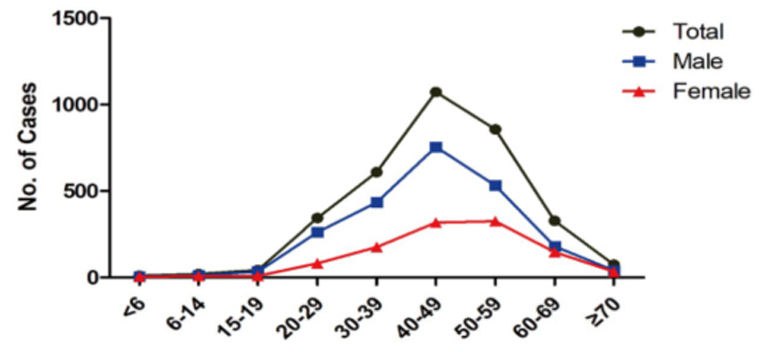
Click the image above to enlarge
Figure 3: Distribution of the occupation of TBE patients over time in China, 2007–201818
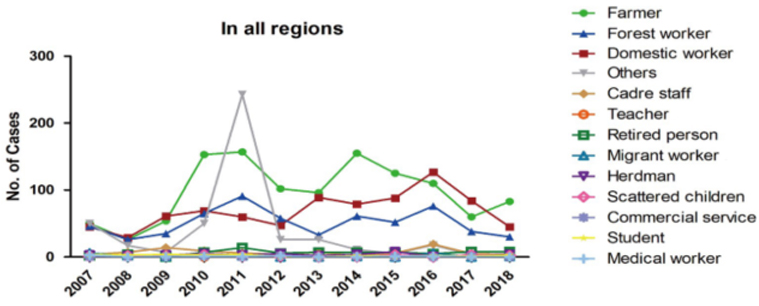
Click the image above to enlarge
Figure 4: Geographic distribution of TBE in China as reported in the published literature4,5
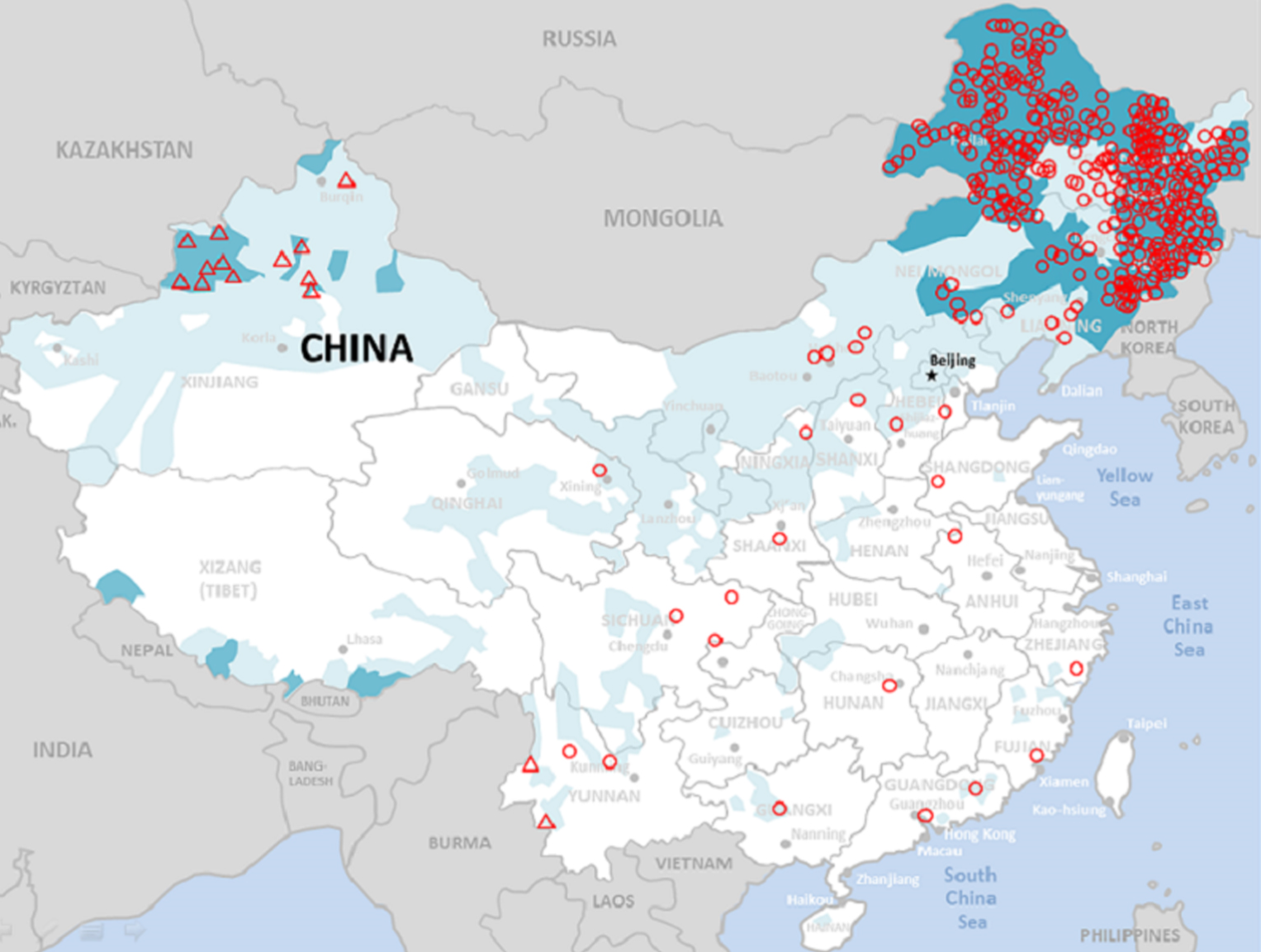
Click the image above to enlarge
Red Triangle: Confirmed TBEV foci in Xinjiang and Yunnan
Intensity of blue color: Reflects the probability of an area to be endemic for TBEV, dark blue = 100%, light blue= lower probabilities based on various criteria as published by Sun et al. 20174
Contact:
Junfeng.yang@pfizer.com
Citation:
Yang J, Schmitt HJ. TBE in China. Chapter 12b. In: Dobler G, Erber W, Bröker M, Schmitt HJ, eds. The TBE Book. 6th ed. Singapore: Global Health Press;2023. doi:10.33442/26613980_12b6-6
References
- Liu YJ, Jiang YT, Guo CS, Guan BP. Epidemiological characteristics of tick-borne encephalitis natural foci in Jilin. Zhongguo Ren Min Jie Fang Jun Jun Shi Yi Xue Ke Xue Yuan Yuan Kan (Bulletin of the Academy of Military Medical Sciences) [in Chinese]. 1979;3:109-20.
- Yin DM, Liu RZ. Review on the control of forest encephalitis in the forest areas of northeast China. Zhonghua Liu Xing Bing Xue Za Zhi (Chinese Journal of Epidemiology) [in Chinese]. 2000;21:387-9.
- Bi WM, Deng HP, Bu XY. Regionalisation of natural foci of forest encephalitis. Shou Du Shi Fan Da Xue Bao (Journal of Capital Normal University: Natural Science Edition) [in Chinese]. 1997;18:100-7.
- Sun RX, Lai SJ, Yang Y, et al. Mapping the distribution of tick-borne encephalitis in mainland China. Ticks Tick Borne Dis. 2017;8:631-9
- Xing Y, Schmitt HJ, Arguedas A, et al. Tick-borne encephalitis in China: A review of epidemiology and vaccines. Vaccine. 2017;35(9):1227-37.
- Huang WL, Hou ZL, Zi DY, Gong ZD, Lei YM, Mi ZQ, et al. Investigation of the Russian Spring-Summer Encephalitis virus in Yunnan province. Zhongguo Yu Fang Shou Yi Xue Bao (Chinese Journal of Preventive Veterinary Medicine) [in Chinese]. 2001;23:231-3.
- Zhang GL, Liu R, Sun X, Zheng Y, Liu XM, Zhao Y, et al. Investigation on the endemic foci of tick-borne encephalitis virus in Xiaerxili Natural Reserve, Xinjiang. Zhonghua Liu Xing Bing Xue Za Zhi (Chinese Journal of Epidemiology) [in Chinese]. 2013;34:438-42.
- Cai ZL, Lu ZX, Hu LM, Zhao ZL, Jin XT, He YY. Epidemiology survey of Russian Spring Summer encephalitis in the northeast area, China. Wei Sheng Wu Xue Za Zhi (Journal of Microbiology) [in Chinese]. 1996;16:19-22.
- Zhang ZQ, Wu YM, Feng L, Wang HJ, Wang LQ, Liu GP, et al. A serological survey of forest encephalitis in northeast of China. Shenyang Bu Dui Yi Yao (Shenyang Army Medical Journal) [in Chinese]. 2006;19:112-3.
- Guo Y. Serological survey of forest encephalitis in Milin, Tibet. Wai Jian Kang Wen Zhai (World Health Digest) [in Chinese]. 2010;7:9-10.
- Zhang DH, Zhang ZX, Wang YM, Wang DH. Trends of forest encephalitis endemic in Heilongjiang. Ji Bing Jian Ce [Disease Surveillance][ in Chinese]. 2000;15:57-8.
- Li H. Analysis of 90 cases of disability as the sequela of forest encephalitis. Lin Chuang Kang Fu (Chinese Journal of Clinical Rehabilitation) [in Chinese]. 2002;6:374.
- Liu R, Zhang G, Liu X, et al. [Detection of the Siberian Tick-borne Encephalitis Virus in the Xinjiang Uygur Autonomous Region, northwestern China]. Bing du xue bao (Chinese Journal of Virology) [in Chinese]. 2016;32(1):26-31.
- He X, Zhao J, Fu S, et al. Complete Genomic Characterization of Three Tick-Borne Encephalitis Viruses Detected Along the China-North Korea Border, 2011. Vector Borne Zoonotic Dis. 2018;18(10):554-559. doi:10.1089/vbz.2017.2173
- Dai X, Shang G, Lu S, Yang J, Xu J. A new subtype of eastern tick-borne encephalitis virus discovered in Qinghai-Tibet Plateau, China. Emerg Microbes Infect. 2018;7(1):74. doi:10.1038/s41426-018-0081-6
- Liu HB. et al. The prevalence and clinical characteristics of tick-borne diseases at One Sentinel Hospital in Northeastern China. Parasitology. 2018;146(2):161-7. doi:10.1017/S0031182018001178
- Deng LQ, Shen B, Li YM. Epidemiology of TBE in Jilin Province from 2010 to 2016. Chin J Biologicals. 2017;30(10):1059-62.
- Chen X, Li F, Yin Q, Liu W, Fu S, He Y, et al. Epidemiology of tick-borne encephalitis in China, 2007- 2018. PLoS ONE. 2019;14(12):e0226712. doi:10.1371/journal.pone.0226712